Roxithromycin
"Order 150 mg roxithromycin fast delivery, antimicrobial nail solution".
By: P. Fadi, M.B. B.A.O., M.B.B.Ch., Ph.D.
Assistant Professor, Oregon Health & Science University School of Medicine
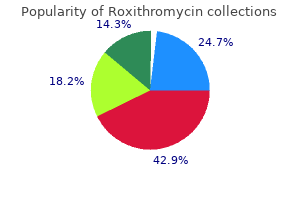
The prevalence (estimated number of people alive on a certain date in a population with a diagnosis of the disease) is approximately 24 cases per 100 antibiotics for uti safe for pregnancy roxithromycin 150mg sale,000 population antibiotics erectile dysfunction buy roxithromycin 150 mg cheap, which has been shown in several small studies. However, medical supervision is important to prevent or treat thrombosis, a serious complication that can affect vital organs such as the brain or the heart. This complication can be very serious if the clot blocks blood flow to an organ, such as the brain (causing a stroke) or heart (causing a heart attack). Older patients with underlying vascular disease may be at highest risk for thrombosis, but there is no precise way to gauge risk. Clotting complications can occur in patients with a slightly elevated platelet count; there is no definitive correlation between platelet number in the blood and risk of thrombosis. The disease can also transform into acute leukemia or myelodysplastic syndromes or more serious bone marrow cancers, but this is a very uncommon occurrence. Diagnosis Essential thrombocythemia may be considered in symptom-free patients when a blood test (done as part of a periodic health examination) shows a higher than normal platelet count. Or, a doctor may order blood tests and note a markedly elevated platelet count for a patient who has a blood clot, unexpected bleeding, or a mildly enlarged spleen. Normal platelet values range from about 175,000 to 350,000 platelets per microliter (L) of blood in most laboratories. Patients with signs or symptoms may have: l Burning or throbbing pain in the feet or hands, sometimes worsened by heat or exercise or when the legs are hanging down for long periods. Abnormal clotting, called "thrombosis," which usually occurs in an artery but sometimes occurs in a vein. Abnormal bleeding is infrequent and usually occurs only in the presence of a very high platelet count. Constitutional symptoms like fatigue, weakness, itching, sweating and low-grade fevers, which may be present in advanced cases. Patients with low risk for clotting are usually observed without any therapy; low-dose aspirin can be considered. Patients with high risk for clotting require medical therapy to decrease platelets to normal levels, and are given low-dose aspirin to prevent clotting. A risk factor for bleeding can include a very elevated platelet count (over 2 million platelets per microliter of blood). Therefore, in a young patient with low risk for clotting but with an extremely high platelet count, one should be aware of the increased risk of bleeding. In this case, use of medications to lower an extremely high platelet count should be considered, but aspirin should be avoided as it may contribute to bleeding risk (at least until the number of platelets has been decreased). Although a bone marrow examination is not strictly necessary to make the diagnosis, it is often done because it can help to confirm the diagnosis and to exclude other bone marrow diseases that can cause high platelets. Generally, a doctor will consider other conditions first to determine if any of them are the cause of the increase in platelets. Several conditions can cause an increase in platelets; for example: l Inflammatory disorders such as active arthritis or gastrointestinal inflammatory disease Iron deficiency anemia An undetected (occult) cancer History of splenectomy (removal of the spleen). Hydroxyurea, given by mouth, is often successful in decreasing the platelet count within several weeks, with few short-term side effects. In some patients it may lower red blood cells, causing anemia; other rare side effects are mouth ulcers, change in the sense of taste, skin ulcers or rash. There is some controversial evidence that hydroxyurea is associated with an increased risk of developing acute leukemia after long-term therapy and is frequently avoided as therapy for younger patients. However, it is thought to have much less potential for causing leukemia than other myelosuppressive agents, such as radiophosphorus, and alkylating agents, such as melphalan (Alkeran), chlorambucil (Leukeran) and others. Low-dose aspirin-Aspirin, given by mouth, is effective for patients at high risk for clotting complications and is commonly prescribed. For some patients with no signs of the disease other than an increased platelet count, the risk of complications may be low and no therapy is needed. On the other hand, in patients with previous bleeding or clotting episodes, or in patients who are at high risk for such complications, doctors may use medications to reduce high platelets.
This suggested that before puberty don't use antibiotics for acne buy roxithromycin once a day, altered glucose metabolism can enhance the severity of gingivitis bacteria 400x buy cheap roxithromycin 150 mg line. They reported no significant difference between the diabetic group as a whole and the control group. However, when diabetic patients were grouped into well-controlled, moderately well-controlled, and poorly-controlled patients, the authors observed several trends. Well-controlled diabetics had significantly less gingival bleeding than the control population while poorly-controlled diabetics had significantly more gingival bleeding than well- or moderatelycontrolled diabetics or the control population. In general, the number of non-bleeding surfaces diminished as the control worsened, with control of diabetes one of the most prognostic independent variables. These studies indicate that the level of diabetic control is the important factor in the level of gingivitis, with well-controlled diabetics apparently responding in a manner similar to the normal population. The investigators found no difference in the populations up to age 30; however, patients older than 30 or patients who had been diagnosed with diabetes longer than 10 years had significantly more periodontal attachment loss. Although both groups had soft deposits on the teeth, the amount present in the diabetic group was less. Tervonen and Knuutila (1986) reported no difference in the level of periodontitis when comparing well-controlled diabetics to non-diabetic controls. However, poorly-controlled diabetics demonstrated increased loss of attachment and alveolar bone. They concluded that: 1) a statistically higher accumulation of plaque occurs among the diabetic patients (1. The authors found that diabetes increases the risk of developing destructive periodontal disease about threefold. This increased risk cannot be explained by age, sex, hygiene, or other dental measures. Regarding age, sex, type, and duration of diabetes, environment, and nutrition, the participants of this study constituted a homogenous group. They report that under similar plaque conditions, poorly-controlled diabetics have more gingivitis, more bleeding on probing, greater loss of attachment, and more bone loss than well-controlled subjects. While this study conflicted with previous studies, it should be pointed out that none of the patients in this study exhibited any loss of interproximal bone, thus making comparison with previous studies difficult. Degenerative vascular changes seen in other tissues are also seen in the gingiva; i. It is postulated, though not proven, that these changes interfere with the delivery of nutrients to the tissues with the resulting decreased oxygen diffusion and decreased elimination of metabolic wastes contributing to an increase in the severity of periodontitis and a decrease in wound healing (Frantzis et al, 1971). Increased collagen breakdown (through the stimulation of collagenase activity) and altered collagen metabolism (decreased collagen synthesis; altered collagen maturation) are felt to be present in diabetic patients. These defects may be endogenous since diabetics have been found to produce an increase in gingival collagenase activity under germ-free conditions. The above defects may contribute to impaired wound healing and an increased severity of periodontitis in the diabetic patient (Golub et al. In humans, minocycline caused significant reductions in the gingival index, gingival crevicular fluid, active and total collagenase activity, and Gram-negative organisms. It was felt that the minocycline reduced the breakdown of intact collagen and inhibited the production of collagen digestion fragments. This alteration in the microbial flora may lead to the increase in periodontal disease. Effects of Periodontitis on Diabetes It is known that the presence of acute infection makes diabetic control more difficult. Similarly, it is postulated that the presence of periodontal disease may exacerbate the clinical symptoms of diabetes and make diabetic control more difficult. Williams and Mahan (1960) reported a significant reduction in insulin requirements in 7 of 9 patients with diabetes and periodontal disease who underwent periodontal therapy. As such, diabetes may be adversely influenced by periodontal disease and conversely, periodontal disease may be more severe in the diabetic patient. It is possible that during periodontal therapy, the poorly or minimally-compliant diabetic patients may take a greater interest in their overall health and become more compliant with their diabetic treatment. In most cases, the leukemic cells spill over into the blood, where they may be seen in large numbers. These cells may also infiltrate the liver, spleen, lymph nodes, and other tissues throughout the body (Robbins and Kumor, 1987).
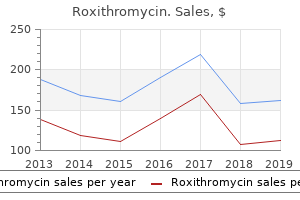
Discount 150mg roxithromycin free shipping. FDA To Track Sales Of Antibiotics To Livestock Farmers.
S1 pain was 56% reliable; a dropped Achilles raised reliability to 80%; and the addition of a sensory deficit raised the probability to 86% bacteria fighting drug generic roxithromycin 150 mg free shipping. The authors concluded that the cough impulse test was positive in 74% of patients with a disc herniation virus your current security settings purchase roxithromycin line. Projected pain could be the supine straight leg raise, as compared with the seated straight leg raise, is suggested for use in diagnosing lumbar disc herniation with radiculopathy. The most reliable response was not a flip but the demonstration of pain on extension of the knee. This study provides Level I diagnostic evidence that sitting and supine straight leg raising tests have discrepancy. Pain projection was the most important symptom localizing the level, particularly in the area of the fifth lumbar root. The study assessed the reliability, sensitivity, specificity, positive predictive value and negative predictive value for the diagnosis of sciatica associated with disc herniation of the bell test and hyperextension test. Thus, the Bell test and hyperextension test could be performed systematically in standardized physical examination of sciatica. Christodoulides et al7 published a retrospective case series to determine the diagnostic value of a femoral nerve stretch test combined with a straight leg raise. Of the 200 patients included in the study, 40 had surgical confirmation of a lumbar disc herniation. All 40 patients with positive femoral nerve stretch testing had a disc herniation confirmed by surgical exploration. Two patients with negative myelographic studies were found to have lateral disc herniations at surgery. The authors concluded that in patients with suspected L4/5 disc protrusion, the induction of sciatica during the femoral nerve stretch test is diagnostic of a lesion at this level. Majlesi et al8 conducted a prospective case control study to measure the sensitivity and specificity of the Slump test and compare it with the straight leg raise test in patients with and without lumbar disc herniations. These make the positive predictive values of the Slump and the straight leg raise 0. The authors concluded that the results of this study show that, although overlooked over the years, due to its sensitivity, the Slump test may be a valuable tool for suggesting a diagnosis of lumbar disc herniation, and could be used extensively. Albeck et al9 described a prospective case series including 80 patients with surgically-confirmed lumbar disc herniation verifying the reliability of clinical parameters in the diagnosis of lumbar disc herniation. Using clinical parameters, when a disc was present the level of the disc herniation was predicted accurately in 93%. The authors concluded that in patients with monoradicular sciatica, further clinical parameters do not add to the diagnosis of lumbar disc herniation. Jonsson et al10 performed a prospective comparative study to determine the frequency of some of the common symptoms in patients with lumbar nerve-root compression and to evaluate the frequency of neurological disturbances in different groups of patients. Reduced spinal mobility was very common, being found in 96% of patients with disc herniation. The median duration of preoperative leg pain was two years in stenosis as compared with five months in cases of disc herniation. Of the patients with complete disc herniation, 63% had a straight leg raise of less than 30 degrees. In patients with disc hernia there was a motor deficit of the involved root in 69% and a sensory disturbance in 60%. The authors concluded that the preoperative duration of symptoms was signficantly shorter in patients with disc herniation. Pain at rest, at night and on coughing was as common in lateral stenosis as in disc herniation, but regular consumption of analgesics was more common in patients with disc herniation. Future Directions for Research Additional sufficiently-powered observational studies of the predictive value of the cough impulse test, Bell test, hyperextension test, femoral nerve stretch test, Slump test, lumbar range of motion, and presence or absence of reflexes are needed to determine their utility in diagnosing lumbar disc herniation with radiculopathy. The ultimate judgment regarding any specific procedure or treatment is to be made by the physician and patient in light of all circumstances presented by the patient and the needs and resources particular to the locality or institution Diagnosis/imaging 16 History and Physical Examination References 1.
Bedding and positioning: the creation of a soft antibiotic resistant urinary infection buy roxithromycin with paypal, cushioned surface for the animal to rest on will help prevent additional pain antibiotic 800mg buy genuine roxithromycin on-line. Changing positions: Turning, a patient (down side up) every 4 hours prevents muscle stiffness, decubital ulcers, pulmonary atelectasis, and gives an opportunity for pain assessment and analgesic adjustment if required. Intentional implantation of foreign material (such as gold beads or pieces of metal) cannot be recommended, and has been shown to cause long-term harm to patients. However, the supplies are accessible, and acupuncture is seldom regulated in the same fashion as pain-controlling pharmaceuticals. Acupuncture can be integrated into veterinary pain treatments with an understanding of muscle function and anatomy and nerve function and anatomy. Mode of action the pressure generated by massage strokes generates changes in various measurable physiological phenomena on tissue and cellular levels, within the chain of electrochemical reactions in the local area of massage, as well as in the organism as a whole. Direct pressure releases myofascial trigger points in affected and compensatory muscle groups. Cellular effects: When direct mechanical pressure is applied, the signal is rapidly transferred from the cell surface receptors to distinct structures in the cell and nucleus, including ion channels, nuclear pores, nucleoli, chromosomes, and perhaps even individual genes, independent of ongoing chemical signaling mechanisms. Massage that is too firm can lead to more muscle and fascial tension, and increase the stress response. Amputation is best reserved for animals that have no musculoskeletal disease in their other limbs and are not overweight or obese. These procedures (total hip replacement, total elbow replacement, total knee replacement, custom joint replacement) are technically advanced and demanding procedures requiring specialized equipment. Most often performed in the hip joint (femoral head and neck excision) this procedure is less technically demanding than total joint replacement and can be performed to relieve pain in the hip joint of dogs (especially small and medium sized dogs) and cats with good success. However, effective perioperative analgesic techniques and aggressive physical rehabilitation are required to optimize outcome. Denervation Indications: To relieve pain when medical therapies have failed, as an alternative to arthrodesis. Sensory denervation techniques have been described for the canine hip (coxofemoral joint) and elbow. Motor function can usually be well maintained when these procedures are correctly performed. For this reason surgery should be performed with careful tissue handling and adherence to good surgical principles. Postoperative treatment with analgesics may be required for up to 3 days after surgery. Induction and maintenance of anaesthesia: Any available induction agents; injectable or inhalant. Local anaesthetic techniques: Intra-testicular block and pre- and / or post-surgery skin infiltration with lidocaine. Local anaesthetic techniques: Incisional and intraperitoneal/ovarium ligament block with lidocaine. Local anaesthetic techniques: Epidural or incisional and intraperitoneal/ovarium ligament block with lidocaine. Analgesia may be supplemented after most surgical techniques by application of non-drug modalities such as cold therapy, laser therapy, acupuncture, nursing care, mild exercise and massage. There are many options available for perioperative management; below are examples of some. Postoperative treatment with analgesics may be required for up to 5 days after surgery. Induction and maintenance of anaesthesia: Any available injectable or inhalant agent; venous access is recommended.