Ropinirole
"Purchase ropinirole 2mg on line, medicine pills".
By: O. Wilson, M.A., M.D., Ph.D.
Co-Director, University of Chicago Pritzker School of Medicine
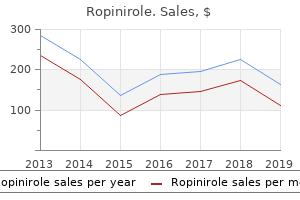
Later in the career symptoms rectal cancer order ropinirole 2mg without a prescription, consequences involving specialty treatment treatment zygomycetes purchase ropinirole 2mg without prescription, hospitalization, and incarceration are more likely to occur. These outcomes are expensive on two counts: once because society incurs costs by addressing the problem xi Comparison of Drug Costs to Other Societal Costs the estimates presented above place illicit drug use on par with other serious chronic health problems in the United States. As was the case here, that study included both direct costs (medical care and services) and indirect costs (short-term and permanent disability as well as premature death). This is driven largely by the fact that obese Americans spend approximately All costs reported in red italics are in thousands. The Economic Impact of Illicit Drug Use on American Society and again because productivity is lost when incapacitation ensues. This points both to the value of providing effective and broadly available specialty treatment and to the value of diverting nonviolent drug users into alternative specialty treatment settings whenever possible. The findings thus validate the basic premises of the National Drug Control Strategy. Strong law enforcement efforts that reduce cultivation, production, and distribution of illicit drugs both limit consumer access and enhance public safety. Prepared communities that support comprehensive local prevention initiatives reduce the probability that individuals will initiate illicit drug use. And a well-developed system of specialty treatment serves ultimately to break the cycle of drug use and criminality. National Institute of Diabetes and Digestive and Kidney Diseases 2008 National Diabetes Statistics, 2007 Factsheet. Department of Health and Human Services, National Institutes of Health, diabetes. Over time, research on the consequences of illicit drug use has become increasingly inclusive, incorporating concepts related to jury compensation (Cohen et al. Prevalence and Incidence-Based Approaches Estimates may be based on the prevalence of a disorder during a given period of time and on the costs associated with treating this disorder during the same period of time or on the incidence of a disorder during a given period of time and on the costs associated with treating this disorder over the entire course of its existence. Given these definitions, it is possible to argue that prior work in this area has employed a mixed model in which some costs have been measured in a manner consistent with a prevalence-based approach while other costs have been measured in a manner consistent with an incidence-based approach. Thus the burden that illicit drug use places on the criminal justice system has been assigned the value of current period costs, while illicit drug-induced premature mortality has been assigned the present discounted value of lifetime earnings. The combination of estimates so derived can produce a distorted picture of the relative magnitude of cost components, and that problem is avoided by adopting a more strictly prevalence-based approach. We believe that this allows a more accurate depiction of the contributions that individual cost components make to the overall cost of illicit drug use. But the refinement renders the estimates provided here and the estimates provided in earlier reports incomparable for lost productivity due to premature mortality and homicide. As an aid to comparison, we provide conventional estimates in these areas as supplemental appendices. Our approach assumes that any number of possible states may be occupied by illicit drug-using individuals. They may be in a jail or prison, in a specialty treatment program or hospital, in the general population, or elsewhere. Presence in these states is episodic, and, at any given moment, the states may be regarded as mutually exclusive. In some cases, societal costs are attributable to an episode of limited duration that falls entirely within the 1-year observation period. When episodes exceed the limits of the observation period, it is necessary to make certain assumptions about the constancy of movement among states during the observation period. Within this context, methods are developed for identifying illicit drug-using individuals and determining whether their criminality, health problems, or reduced productivity is attributable to illicit drug use. When estimating criminal justice system costs, information provided by prisoners regarding the circumstances of their crime is examined in order to render an assessment of whether it was actually induced by illicit drug use.
As with the pharmacological treatments for sleep disturbances symptoms jaw bone cancer order 2mg ropinirole, more research is needed to determine if these strategies will help improve insomnia in individuals with other substance use disorders as well symptoms zika virus purchase generic ropinirole on-line. In community population samples studied in the National Comorbidity Survey (341), individuals with alcohol dependence had high rates of clinically significant depression during their lifetime (men: 24% depression and 11% dysthymia; women: 49% depression and 21% dysthymia). Individuals with bipolar disorder had high rates of alcohol (61%) and other substance (41%) dependence (342). In substance use disorder treatment settings, depression, anxiety, and personality disorders frequently occur. Individuals with nicotine dependence are more likely to have co-occurring psychiatric disorders than the general U. One analysis of nicotine use as reported in the National Comorbidity Survey found that individuals with psychiatric disorders were about twice as likely to smoke as the general population and that about 44% of the cigarettes smoked in the United States were smoked by individuals with a psychiatric disorder (349). Use of multiple substances and co-occurring psychiatric and substance use disorders are now so common in treatment settings that these combinations should be expected. Thus, all patients with a substance use disorder should be carefully assessed for the presence of co-occurring psychiatric disorders, including additional substance use disorders. Conversely, patients with identified psychiatric disorders should be routinely assessed for the presence of a co-occurring substance use disorder (350, 351). Treating individuals with co-occurring psychiatric and substance use disorders in traditional inpatient and outpatient programs is challenging. Recent research and consensus opinions by experts in the field support the notion that the integration of substance abuse and mental health treatment strategies, including integrated systems, programs, and clinical treatment, improves patient outcome (80, 121, 352, 353). Integrated treatment usually requires incorporating and modifying traditional psychiatric and substance abuse treatment methods so that the co-occurring disorders receive simultaneous treatment. Integrated treatment Recent research and clinical experience (80, 288) has also shed light on the question of treatment timing. The integrated treatment of co-occurring psychiatric and substance use disorders can include psychosocial and/or pharmacological interventions. Initial treatment efforts should include engaging the patient in treatment and assessing and managing the most severe symptoms of both types of disorders. When patients are being treated in a substance abuse treatment setting, their psychiatric symptoms should be monitored and addressed clinically through psychiatric medications, when appropriate, as well as through integrated psychosocial strategies. Treatment of Patients With Substance Use Disorders 49 Copyright 2010, American Psychiatric Association. In a psychiatric treatment setting, it would be incorrect to assume that successful treatment of a psychiatric disorder will resolve the substance use disorder. The substance use disorder will require specific treatment even when it arises in the context of another psychiatric disorder, a situation that is quite common and that presents an opportunity for the prevention of a secondary disorder (358). Certain psychosocial and pharmacological treatments have been studied for specific combinations of psychiatric and substance use disorders. Pharmacological management of psychiatric disorders In most patients, the same medications are recommended for the treatment of a specific psychiatric disorder whether that disorder co-occurs with a substance use disorder or not. Clinical issues such as medication tolerability, safety, and abuse potential are important considerations in choosing a medication and will influence traditional psychopharmacological treatment algorithms. There is no evidence to suggest that the duration of pharmacotherapy for a psychiatric disorder in conjunction with a co-occurring substance use disorder would differ from that needed to treat the psychiatric condition alone, and there are no data to suggest that decisions about continuation and maintenance treatment should differ (288). An important clinical question in treating a co-occurring psychiatric disorder in a substance use disorder treatment setting is whether the prescribing clinician should initiate psychiatric medications during the acute treatment of the substance use disorder. If there is little overlap between the symptoms observed and the expected abstinence syndrome (such as bulimia nervosa in an opioid-dependent patient), then the psychiatric diagnosis can be immediately established. Medication nonadherence is common among individuals with co-occurring psychiatric and substance use disorders (359, 360). When such medications are necessary, a clinician should prescribe them with caution and closely monitor their use.
Improving the Quality of Health Care for Mental and Substance Use Conditions also discussed the shortage of skills both in specialty substance use disorder programs and in the general health care system treatment 001 ropinirole 0.5mg fast delivery. Workforce Development and Improvement the Annapolis Coalition on the Behavioral Health Workforce provided a framework for workforce development in response to the challenges described above symptoms hypoglycemia order ropinirole line,318 focusing on broadening the definition of "workforce" to address needed changes to the health care system. Currently, 66 organizations license and credential addiction counselors,319,320 and although a consensus on national core competencies for these counselors exists,321 they have not been universally adopted. Credentialing for prevention specialists exists through the International Certification & Reciprocity Consortium,322,323 but core competencies for prevention professionals have not been developed. Without a comprehensive, coordinated, and focused effort, workforce expansion and training will continue to fall short of the challenge of meeting the needs of individuals across the continuum of service settings. Of particular note is the National Health Service Corps, where, as of September 2015, roughly 30 percent of its field strength of 9,683 was composed of behavioral health providers, meeting service obligations by providing care in areas of high need. Protecting Confidentiality When Exchanging Sensitive Information Effectively integrating substance use disorder treatment and general health care requires the timely exchange of patient health care information. In the early 1970s, the federal government enacted Confidentiality of Alcohol and Drug Abuse Patient Records (42 U. These privacy protections were motivated by the understanding that discrimination attached to a substance use disorder might dissuade people from seeking treatment, and were enacted in the context of patient methadone records being used in criminal cases. Given the long and continuing history of discrimination against people with substance use disorders, safeguards against inappropriate or inadvertent disclosures are important. Disclosures to insurers or to employers can render patients unable to obtain disability or life insurance and can cost patients their jobs. However, exchanging treatment records among health care providers has the potential to improve treatment and patient safety. For example, in the case of opioid prescribing, a study in health systems of long-term opioid users found those with a prior substance use disorder diagnosis received higher dosages and were co-prescribed sedative-hypnotic medications-which can increase the risk for overdose-more often. Promising Innovations That Improve Access to Substance Use Disorder Treatment Clearly, integrating health care and substance use disorder treatment within health care systems, as well as integrating the substance use disorder treatment system with the overall health care system, are complex undertakings. In so doing, they are broadening the focus of interventions beyond just the treatment of severe substance use disorders to encompass the entire spectrum of prevention, treatment, and recovery. Medicaid Innovations Medicaid is not only an increasing source of financing for substance use disorder treatment services, it has become an important incubator for innovative substance use disorder financing and delivery models that can help integrate substance use disorder treatment and mainstream health care systems. These services include therapy, counseling, training in communication and independent living skills, recovery support and relapse prevention training, skills training to return to employment, and relationship skills. Nearly all states offer some rehabilitative mental health services, and most states offer the rehabilitation option for substance use disorder services. The agency is providing technical and program support to states to introduce policy, program, and payment reforms to identify individuals with substance use disorders, expand coverage for effective treatment, expand access to services, and develop data collection, measurement, and payment mechanisms that promote better outcomes. Health Homes Health homes are grounded in the principles of the primary care medical home, which focuses on primary care-based coordination of diverse health care services, and patient and provider engagement. The Affordable Care Act created an optional Medicaid State Plan benefit allowing states to establish health homes to coordinate care for participants who have chronic health conditions. Beneficiaries with chronic conditions are eligible to enroll in health homes if they experience (or are at risk for) a second chronic condition, including substance use disorders, or are experiencing serious and persistent mental health conditions. These arrangements emphasize integration of care, targeting of health home services to high-risk populations with substance use and mental health concerns, and integration of social and community supports with general health services. The Oregon Health Authority publishes regular reports on quality, access, and progress toward benchmarks in both prevention and treatment. Federally Qualified Health Centers Increased insurance coverage and other provisions of the Affordable Care Act have sparked important changes that are facilitating comprehensive, high-quality care for people with substance use disorders. These community health centers emphasize coordinated primary and preventive services that promote reductions in health disparities for low-income individuals, racial and ethnic minorities, rural communities, and other underserved populations. Community health centers provide primary and preventive health services to medically underserved areas and populations and may offer behavioral and mental health and substance use services as appropriate to meet the health needs of the population served by the health center. Because they provide services regardless of ability to pay and are required to offer services on a sliding scale fee, they are well-positioned to serve low-income and economically vulnerable patients. These systems have the capacity to easily provide information in multiple languages and to put patients in touch with culturally appropriate providers through telehealth. A system to providers, and they can support care coordination by that provides health care professionals, staff, patients, or other individuals facilitating communications between primary and specialty with knowledge and person-specific care providers across health systems.
If a program has a reputation for providing effective care symptoms ruptured ovarian cyst buy on line ropinirole, then managed care enrollees and other potential clients will want to use it treatment wpw purchase cheapest ropinirole. Effective substance abuse treatment provided promptly may reduce medical care and hospitalization costs in the long run. Of course, the Financing and Organizational Issues 167 skills and connections that will advance the purposes of the detoxification program. However, consultation with an attorney is strongly advised prior to developing such a coalition or other collaboration with local treatment providers as the laws regarding antitrust and other matters related to such relationships are complex. Preparing for the Future Major forces that shape and limit provider financing are unlikely to change substantially in the near future. Careful strategic planning and assurance of funding from reputable and varied referral sources are essential for new and existing programs. As a buffer against shrinking budgets, all programs should con sider broadening their funding streams and referral sources, expanding the range of clients they can serve, and promptly referring clients for other services not provided on site. To operate effectively, administrators and other staff must thoroughly understand the managed care and community political environment including its terminology, contracts, negotia tions, payments, appeals, and priority popu lations. Traditional and Western healing practices for alcoholism in American Indians and Alaska Natives. Electrocardiographic abnormalities during recovery from ultrashort opiate detoxifi cation. Counseling the Hispanic client: Cuban Americans, Mexican Americans, and Puerto Ricans. Depressive mood and craving during alcohol withdrawal: Association and interaction. Public hospi tals and substance abuse services for preg nant women and mothers: Implications for managedcare programs and Medicaid. Carbohydratedeficient transfer rin for detection and monitoring of sus tained heavy drinking. A double blind comparison of abecarnil and diazepam in the treatment of uncomplicat ed alcohol withdrawal. Predictors of discharges against medical advice from a shortterm hospital detoxification unit. The role of social anxiety in matching methadone patients to psychosocial treatments. Psychotherapy of adults with comorbid attention deficit hyperactivity disorder and psychoactive substance use disorder. Position of the American Dietetic Association: Nutrition intervention in treatment and recovery from chemical dependency. Predicting length of stay of substance using pregnant and postpartum women in day treatment. Cardiovascular toxicity of nicotine: Implications for nicotine replacement ther apy. Slower metabolism and reduced intake of nicotine from cigarette smoking in ChineseAmericans. Sources of variability in nicotine and coti nine levels with use of nicotine nasal spray, transdermal nicotine, and cigarette smoking. A clinical trial of buprenor phine: Comparison with methadone in the detoxification of heroin addicts. Psychiatric symptoms in alco hol dependence: Diagnostic and treatment implications. Nicotine nasal spray with nicotine patch for smoking cessation: Randomised trial with six year follow up. Transmission of tuberculosis in San Francisco and its association with immi gration and ethnicity.
The physician should consider intramus cular or intravenous haloperidol (Haldol and others) to treat agitation and hallucinations 5 asa medications order ropinirole now. Nursing care is vital medications prednisone purchase ropinirole 1 mg overnight delivery, with particular attention to medication administration, patient comfort, soft restraints, and frequent contact with ori enting responses and clarification of environ mental misperceptions. The majority of alcohol withdrawal seizures occur within the first 48 hours after cessation or reduction of alcohol, with peak incidence around 24 hours (Victor and Adams 1953). Most alcohol withdrawal seizures are singular, but if more than one occurs they tend to be within several hours of each other. While alcohol withdrawal seizures can occur several days out, a higher index of suspicion for other causes is prudent. The occurrence of an alcohol withdrawal seizure happens quickly, usually without warn ing to the individual experiencing the seizure or anyone around him. The patient loses con sciousness, and if seated usually slumps over, but if standing will immediately fall to the floor. This part of the seizure is called the tonic phase, which usually lasts for a few seconds and rarely more than a minute. The next part of the seizure (more dramatic and generally remembered by witnesses) con 64 sists of jerking of head, neck, arms, and legs. Immediately after the jerking ceases, the patient generally has a period of what appears to be sleep with more regular breathing. Rarely, the patient may appear not to waken at all and have a second period of rigidity followed by muscle jerking. Upon awakening, the individual usually is mildly confused as to what has happened and may be disoriented as to where she or he is. This period of postseizure confusion generally lasts only for a few minutes but may persist for several hours in some patients. Headache, sleepiness, nausea, and sore muscles may per sist in some individuals for a few hours. Patients who start to retch or vomit should be gently placed on their side so that the vomitus (stomach contents vomited) may exit the mouth and not be taken into the lungs. Predicting who will have a seizure during alco hol withdrawal cannot be accomplished with any great certainty. There are some factors that clearly increase the risk of a seizure, but even in individuals with all of these factors, most patients will not have a seizure. Out of 100 people experiencing alcohol withdrawal only two or three of them will have a seizure. The best single predictor of a future alcohol withdrawal seizure is a previous alcohol with drawal seizure. Individuals who have had three or more documented withdrawal episodes in the past are much more likely to have a seizure regardless of other factors including age, gen der, or overall medical health. Such attempts at object insertion may cause damage to the teeth and tongue, or objects may get partially swallowed and obstruct the airway. Vomitus taken into the lungs is a severe medical condition leading to immediate difficulty breathing and, within hours, severe pneumonia. In the rare patient with recurrent multiple seizures or status epilepticus (continuous seizures of sever al minutes) an anesthesiology consultation may be required for general anesthesia. Despite this report, the consensus panel agrees that hospi talization for further detoxification treatment is strongly advised to monitor and ameliorate other withdrawal symptoms, reduce suffering, and stabilize the patient for rehabilitation treatment. Further evaluation of a first seizure often warrants neurologic evaluation (com puterized tomography and electroencephalo gram), even if the seizure may be suspected to have been due to alcohol withdrawal. Patient Care and Comfort Interpersonal support and hygienic care along with adequate nutrition should be provided. Staff assisting patients in detoxification should provide whatever assistance is necessary to help get patients cleaned up after entering the facility and bathed thoroughly as soon as they have been medically stabilized. Attention to the treatment of scabies, body lice, and other skin conditions should be given.
Purchase ropinirole 0.5 mg. Sad Quotes and Sayings about Life.