Himplasia
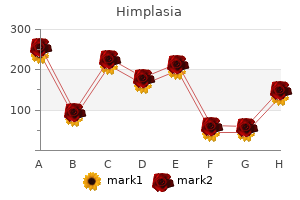
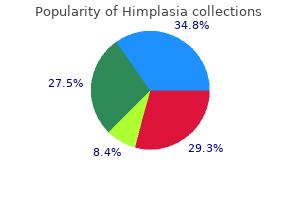
"Order himplasia with mastercard, 101 herbals".
By: E. Porgan, M.B. B.A.O., M.B.B.Ch., Ph.D.
Vice Chair, University of Central Florida College of Medicine
The less active patient can be kept in bed by side rails herbals on demand shipping discount himplasia 30caps, wrist restraints herbs to lower blood pressure purchase himplasia 30 caps visa, or a restraining sheet or vest. The fully awake but confused patient should be permitted to sit up or walk about the room part of the day unless this is contraindicated by the primary disease. All drugs that could possibly be responsible for the acute confusional state or delirium should be discontinued if this can be done safely. These include sedating, antianxiety, narcotic, anticholinergic, antispasticity, and corticosteroid medications, L-dopa, metoclopramide (Reglan), and cimetidine (Tagamet) as well as antidepressants, antiarrhythmics, anticonvulsants, and antibiotics. Despite the need to be sparing with medications in these circumstances, haloperidol, quetiapine, and risperidone are helpful in calming the agitated and hallucinating patient, but they too should be used in the lowest effective doses. An exception is alcohol or sedative withdrawal, in which chlordiazepoxide (Librium) is the treatment favored by most physicians, but chloral hydrate (difficult to obtain), lorazepam, and diazepam are trustworthy and equally effective sedatives if given in full doses (see Chap. In delirious patients, the purpose of sedation is to assure rest and sleep, avoid exhaustion, and facilitate nursing care, but one must be cautious in attempting to suppress delirium completely. Warm baths were also known to be effective in quieting the delirious patient, but few hospitals have facilities for this valuable method of treatment. It would seem obvious that attempts should be made to preempt the problem of confusion in the hospitalized elderly patient (beclouded dementia). Inouyue and colleagues have devised an intervention program that includes frequent reorientation to the surroundings, mentally stimulating activities, ambulation at least three times a day or similar exercises when possible, and attention to providing visual and hearing aids in patients with these impairments. They recorded a 40 percent reduction in the frequency of a confusional illness in comparison to patients who did not receive this type of organized program. Preventive strategies of the type they outline are most important in the elderly, even those without overt dementia, but a routine plan must be made so that nurses and ancillary staff are able to assiduously apply them. Finally, the physician should be aware of the benefit of many small therapeutic measures that allay fear and suspicion and reduce the tendency to hallucinations. The room should be kept dimly lighted at night and, if possible, the patient should not be moved from one room to another. Every procedure should be explained to the patient, even such simple ones as the taking of blood pressure or temperature. The presence of a member of the family may help the patient to maintain contact with reality. It may be some consolation and also a source of professional satisfaction to remember that most confused and delirious patients recover if they receive competent medical and nursing care. The family should be reassured on this point but forewarned that improvement may take several days or more. This may indicate the development of a degenerative brain disease, a brain tumor, multiple strokes, a chronic subdural hematoma, chronic drug intoxication, chronic meningoencephalitis (such as caused by acquired immunodeficiency syndrome or syphilis), normal-pressure hydrocephalus, or a depressive illness. Formerly, when there was little that could be done about these clinical states, no great premium was attached to diagnosis. But modern medicine offers the means of treating several of these conditions and in some instances of restoring the patient to normal mental competence. This topic should be of interest to neurologists because intelligence is disturbed by many disorders of the brain but cannot be easily attributed to any cerebral region or particular cognitive function. Moreover, in the dementias and in mental retardation, intelligence is greatly affected in a way that cannot be explained except by some unique but global aspect of brain function. As every educated person knows, intelligence has something to do with normal cerebral function. It is also apparent that the level of intelligence differs widely from one person to another, and members of certain families are exceptionally bright and intellectually accomplished, while members of other families are just the opposite. If properly motivated, intelligent children excel in school and score high on intelligence tests. Indeed, the first intelligence tests, devised by Binet and Simon in 1905, were for the purpose of predicting scholastic success. At any given age a large sample of normal children attain test scores that range in conformity with the normal or Gaussian distribution.
These episodes of mydriasis herbs not to mix purchase 30 caps himplasia overnight delivery, which are more common in women 18 herbals purchase himplasia 30 caps with amex, last for minutes to days and may recur at random intervals. Oculomotor palsies and ptosis are notably lacking, but sometimes the pupil is distorted during the attack. Some patients complain of blurred vision and head pain on the side of the mydriasis, suggesting an atypical form of ophthalmoplegic migraine. In children, following a minor or major seizure, one pupil may remain dilated for a protracted period of time. The main consideration in an awake patient is that the cornea has inadvertently (or purposefully) been exposed to mydriatic solutions, among them vasopressor agents used in cardiac resuscitation. As stated above, in dealing with anisocoria, it is worth noting that at any given examination, 20 percent of normal persons show an inequality of 0. This is "simple" or physiologic anisocoria, and it may be a source of confusion in patients with small pupils. Its main characteristic is that the same degree of asymmetry in size is maintained in low, ambient, and bright light conditions. It is also variable from day to day and even from hour to hour and often will have disappeared at the time of the second examination (Loewenfeld; Lam et al). In first dealing with the problem of pupillary asymmetry, one has to determine which of the pupils is abnormal. If it is the larger one, the light reaction will be muted on that side; if it is the smaller pupil, it will fail to enlarge in response to shading both eyes. More simply stated, light exaggerates the anisocoria due to a third-nerve lesion, and darkness accentuates the anisocoria in the case of a Horner syndrome. A persistently small pupil always raises the question of a Horner syndrome, a diagnosis that may be difficult if the ptosis is slight and facial anhidrosis undetectable. In darkness, the Horner pupil dilates more slowly and to a lesser degree than the normal one because it lacks the pull of the dilator muscle (dilation lag). The diagnosis can be confirmed by placing 1 or 2 drops of 2 to 10% cocaine in each eye; the Horner pupil dilates not at all or much less than the normal one- a response that can be documented by photos taken after 5 and 15 s of darkness. Such a response to cocaine will occur with a defect at any point along the sympathetic pathway (page 461) because lesions of the first- or second-order sympathetic neurons eventually deplete norepinephrine at the synapses with third-order neurons. The reduction of neurotransmitter at the nerve endings in the ciliary dilator muscle greatly reduces the reuptake blocking effects of cocaine. If the subsequent (24 h after cocaine) application of the adrenergic mydriatic hydroxyamphetamine (1%) has no effect, the lesion can be localized to the postganglionic portion of the pathway since this drug releases any norepinephrine that may remain in the third-order neuron. Localization of the lesion to the central or preganglionic parts of the sympathetic pathway depends upon the associated symptoms and signs (Chap. A variety of lesions, some of them purely ocular, such as uveitis, may give rise to a dilated pupil. Neurologically, there are three main diagnostic considerations: An interruption of the parasympathetic preganglionic pupilloconstrictor fibers in the third nerve. It is a safe clinical rule that the interruption of these fibers is practically always associated with ptosis, palsy of the extraocular muscles, or signs of other brainstem or cerebral disease. The importance of unilateral pupillary enlargements in the diagnosis of coma is discussed in Chap. Often in this circumstance the pupil goes through an early phase of miosis followed by irregularly shaped enlargement. Here one requires that the pupillary abnormalities conform to the diagnostic criteria for this disorder, enumerated above. Not infrequently, particularly among nurses and pharmacists, a mydriatic fixed pupil is the result of accidental or deliberate application of an atropinic or sympathomimetic drug. Failure of 1% pilocarpine drops to contract the pupil provides proof that the iris sphincter has 1. Differential Diagnosis of Anisocoria In regard to pupillary disorders, there are two main issues with which the neurologist has to contend. One is the problem of unequal pupils (anisocoria) and determining whether this abnormality is derived from sympathetic or parasympathetic denervation. Completely Sector palsy immobile of iris Test for cholinergic sphincter Impaired No dilation lag ``Dilation lag' supersensitivity with light reaction of smaller Mecholyl 2. As a rule, bilateral smallness of pupils does not pose a difficult diagnostic problem.
Impairment of visual acuity evolves over several days or a week or two goyal herbals private limited order 30caps himplasia with mastercard, and examination discloses bilateral herbals dario discount himplasia 30 caps overnight delivery, roughly symmetrical central or centrocecal scotomas, the peripheral fields being intact. With appropriate treatment (nutritious diet and B vitamins) instituted soon after the onset of amblyopia, complete recovery is possible; if treatment is delayed, patients are left with varying degrees of permanent defect in central vision and pallor of the temporal portions of the optic discs. This disorder has commonly been referred to as "tobacco-alcohol amblyopia," the implication being that it is due to the toxic effects of tobacco or alcohol, or both. In fact, the disorder is one of nutritional deficiency and is more properly desig- Figure 13-12. There is diffuse disc swelling from infarction that extends into the retina as a milky edema. The same disorder may be seen under conditions of severe dietary deprivation (Strachan syndrome, page 992) and in patients with vitamin B12 deficiency (page 994). Another cause is Leber hereditary optic atrophy, an inherited disorder of mitochondria, a subject that is reviewed by Newman and discussed in Chap. Subacute optic neuropathy of possible toxic origin has been described in Jamaican natives. It is characterized by a bilaterally symmetrical central visual loss and may have additional features of nerve deafness, ataxia, and spasticity. A similar condition has been described in other Caribbean countries, most recently in Cuba, where an optic neuropathy of epidemic proportions was associated with a sensory polyneuropathy. A nutritional etiology, rather than tobacco use (putatively, cigars in the Cuban epidemic), is likely but has not been proved conclusively (see Sadun et al and the Cuba Neuropathy Field Investigation report). Impairment of vision due to methyl alcohol intoxication (methanol) is abrupt in onset and characterized by large symmetrical central scotomas as well as symptoms of systemic disease and acidosis. The subacute development of central field defects has also been attributed to other toxins and to the chronic administration of certain therapeutic agents: halogenated hydroxyquinolines (clioquinol), chloramphenicol, ethambutol, isoniazid, streptomycin, chlorpropamide (Diabinese), inflixamab, and various ergot preparations. The main drugs reported to have a toxic effect on the optic nerves are listed in Table 13-3 and have been catalogued by Grant. Developmental Abnormalities Congenital cavitary defects due to defective closure of the optic fissure may be a cause of impaired vision because of failure of development of the papillomacular bundle. Usually the optic pit or a larger coloboma is unilateral and unassociated with developmental abnormalities of the brain (optic disc dysplasia and dysplastic coloboma). Vision may also be impaired as a result of developmental anomalies of the optic nerves; the discs are of small diameter (hypoplasia of the optic disc or micropapilla). Toxins and drugs Methanol Ethambutol Chloroquine Streptomycin Chlorpropamide Chloramphenicol Infliximab Ergot compounds, etc. Radiation-induced optic neuropathy Other Optic Neuropathies Optic nerve and chiasmal involvement by gliomas, meningiomas, craniopharyngiomas, and metastatic tumors (most often from lung or breast) may cause scotomas and optic atrophy (Chap. Pituitary tumors characteristically cause bitemporal hemianopia, but very large adenomas, in particular if there is pituitary apoplexy, can cause blindness in one or both eyes (see page 577). Of particular importance is the optic nerve glioma that occurs in 15 percent of patients with type I von Recklinghausen neurofibromatosis. Usually it develops in children, often before the fourth year, causing a mass within the orbit and progressive loss of vision. If the eye is blind, the recommended therapy is surgical removal to prevent extension into the optic chiasm and hypothalamus. If vision is retained, radiation and chemotherapy are the recommended forms of treatment. Thyroid ophthalmopathy with orbital edema, exophthalmos, and usually a swelling of extraocular muscles is an occasional cause of optic nerve compression. Anderson Cancer Center who received radiotherapy for carcinomas of the nasal or paranasal region, retinopathy occurred in 7, optic neuropathy with blindness in 8, and chiasmatic damage with bilateral visual impairment in 1. These complications followed the use of more than 50 Gy (5000 rad) of radiation (see Jiang et al). Finally, it should be mentioned again that long-standing papilledema from any cause may eventually lead to optic atrophy and blindness. In the case of pseudotumor cerebri, the visual loss may be unexpectedly abrupt, appearing in a day or less and even sequentially in both eyes. This seems to happen most often in patients with constitutionally small optic nerves, no optic cup of the nerve head, and, presumably, a small aperture of the lamina cribrosa. Thus the visual cortex receives a spatial pattern of stimulation that corresponds with the retinal image of the visual field.
When the details of such cases become known herbals usa cheap 30 caps himplasia with mastercard, it is evident that recovery might reasonably have been expected herbs used for pain himplasia 30caps without prescription. There are, however, numerous reported instances of partial recovery in patients- particularly children- who display vegetative features for several weeks or, as Andrews describes, even several months after injury. Such observations cast doubt on unqualified claims of success with various therapies, such as sensory stimulation. Nevertheless, the occurrence of rare instances of very late recovery in adults must be acknowledged [see Andrews; Higashi et al; and Rosenberg et al (1977)]. The term pseudocoma as a synonym for this state is best avoided, since it is used by some physicians to connote the feigned unconsciousness of the hysteric or malingerer. The locked-in syndrome is due most often to a lesion of the ventral pons (basis pontis) as a result of basilar artery occlusion. Such an infarction spares both the somatosensory pathways and the ascending neuronal systems responsible for arousal and wakefulness as well as certain midbrain elements that allow the eyelids to be raised and give the appearance of wakefulness; the lesion essentially interrupts the corticobulbar and corticospinal pathways, depriving the patient of speech and the capacity to respond in any way except by vertical gaze and blinking. One could logically refer to the locked-in state as akinetic mutism insofar as the patient is akinetic (motionless) and mute, but this is not the sense in which the term was originally used by Cairns and colleagues. They described a patient who appeared to be awake but was unresponsive (actually their patient was able to answer in whispered monosyllables). This rare state of apparent vigilance in an imperceptive and unresponsive patient has been referred to by French authors as coma vigile, but the same term has been applied to the vegetative state. The term akinetic mutism has been applied to yet another group of patients who are silent and inert as a result of bilateral lesions of the anterior parts of the frontal lobes, leaving intact the motor and sensory pathways; the patient is profoundly apathetic, lacking to an extreme degree the psychic drive or impulse to action (abulia) (pages 359 and 394). The psychiatric patient with catatonia appears unresponsive, in a state that simulates stupor, light coma, or akinetic mutism. There are no signs of structural brain disease, such as pupillary or reflex abnormalities. There is usually resistance to eye opening, and some patients display a waxy flexibility of passive limb movement that gives the examiner a feeling of bending a wax rod (flexibilitas cerea); there is also the retention for a long period of seemingly uncomfortable limb postures (catalepsy). Peculiar motor mannerisms or repetitive motions, seen in a number of these patients, may give the impression of seizures; choreiform jerking has also been reported, but the latter sign should suggest the possibility of seizure activity. Since there is considerable imprecision in the use of terms by which these states are designated, the physician would be better advised to supplement designations such as coma and akinetic mutism by simple descriptions indicating whether the patient appears awake or asleep, drowsy or alert, aware or unaware of his surroundings, and responsive or unresponsive to a variety of stimuli. This requires that the patient be observed more frequently or over a longer period than the several minutes usually devoted to this portion of the neurologic examination. Brain Death In the late 1950s European neurologists called attention to a state of coma in which the brain was irreversibly damaged and had ceased to function but pulmonary and cardiac function could still be maintained by artificial means. Mollaret and Goulon referred to this condition as coma depasse (a state beyond coma). The concept that a person is dead if the brain is dead and that death of the brain may precede the cessation of cardiac function has posed a number of important ethical, legal, and social problems as well as medical ones. The various aspects of brain death have since been the subject of close study by several professional committees, which have for the most part confirmed the 1968 guidelines for determining that the brain is dead. The monograph by our colleague Wijdicks is a thorough and modern source on the subject of brain death and also addresses the subject from an international perspective. The central considerations in the diagnosis of brain death are (1) absence of cerebral functions; (2) absence of brainstem functions, including spontaneous respiration; and (3) irreversibility of the state. Following from the last criterion, it is necessary to demonstrate an irrefutable cause of the catastrophic brain damage. The absence of cerebral function is judged by the presence of deep coma and total lack of spontaneous movement and of motor and vocal responses to all visual, auditory, and cutaneous stimulation. Spinal reflexes may persist in some cases, and the toes often flex slowly in response to plantar stimulation; but a well-developed Babinski sign is unusual in our experience (although its presence does not exclude the diagnosis of brain death). Extensor or flexor posturing is seen from time to time as a transitional phenomenon just after brain death becomes evident. The absence of brainstem function is judged by the loss of spontaneous eye movements, midposition of the eyes, and lack of response to oculocephalic and caloric (oculovestibular) testing; presence of dilated or midposition fixed pupils (not smaller than 3 mm); paralysis of bulbar musculature (no facial movement or gag, cough, corneal, or sucking reflexes); an absence of motor and autonomic responses to noxious stimuli; and absence of respiratory movements.
Generic himplasia 30caps amex. Herbalism Certificate Program at Denver Botanic Gardens.