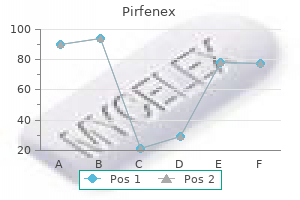
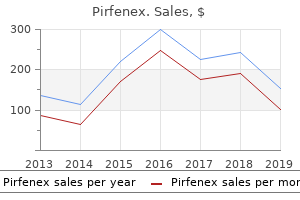
Pirfenex
"Cheap pirfenex online, medicine identification".
By: H. Dolok, MD
Associate Professor, Medical College of Georgia at Augusta University
Pulmonary stenosis results from the failure of the development medicine the 1975 cheap pirfenex 200mg without prescription, in early gestation medications for ptsd proven pirfenex 200mg, of the three leaflets of the valve, insufficient resorption of infundibular tissue, or insufficient canalization of the peripheral pulmonary arteries. Failure of the septum to fuse with the endocardial cushion results in abnormal atrioventricular valves as well. In addition to left-to-right shunting at both levels, there may be atrioventricular valve insufficiency. Newborns with severe stenosis may be more symptomatic and even cyanotic because of right-to-left shunting at the atrial level. Pulmonary stenosis causes a systolic ejection murmur at the second left intercostal space which radiates to the back. With more severe pulmonary stenosis, an impulse at the lower left sternal border results from right ventricular hypertrophy. Worsening stenosis causes an increase in the duration of the murmur and a higher frequency of the sound. The systolic ejection murmurs of peripheral pulmonary ste nosis are heard distal to the site of obstruction in the pulmonary circulation, including radiation to the back. Clinical Manifestations Imaging Tests Clinical Manifestations the symptoms of heart failure usually develop as the pulmonary vascular resistance decreases over the first 6 to 8 weeks of life. Moderate to severe stenosis results in right axis deviation and right ventricular hypertrophy. The heart size is usually normal on chest x-ray, although dilation of the main pulmonary artery may be seen. Echocardiography provides assessment of the site of stenosis, degree of hypertrophy, and valve morphology, as well as an estimate of the pressure gradient. During development of the aortic arch, the area near the insertion of the ductus arteriosus fails to develop correctly, resulting in a narrowing of the aortic lumen. Treatment Valvular pulmonary stenosis usually does not progress, especially if it is mild. Balloon valvuloplasty is usually successful in reducing the gradient to acceptable levels for more significant or symptomatic stenosis. Surgical repair is required if balloon valvuloplasty is unsuccessful or when subvalvular (muscular) stenosis is present. Lesions result from failure of development of the three leaflets or failure of resorption of tissue around the valve. More severe stenosis results in easy fatigability, exertional chest pain, and syncope. A systolic ejection murmur is heard at the right second intercostal space along the sternum and radiating into the neck. The murmur increases in length and becomes higher in frequency as the degree of stenosis increases. With valvular stenosis, a systolic ejection click often is heard, and a thrill may be present at the right upper sternal border or in the suprasternal notch. Dilation of the ascending aorta or aortic knob due to an intrinsic aortopathy may be seen on chest radiographs. Echocardiography shows the site of stenosis, valve morphology, and the presence of left ventricular hypertrophy, and it allows an estimate of the pressure gradient. Imaging Studies Timing of presentation depends on the severity of obstruction and associated cardiac defects. They may be dependent on a patent ductus arteriosus to provide descending aortic flow. Symptoms, including poor feeding, respiratory distress, and shock, may develop before 2 weeks of age. Classically the femoral pulses are weaker and delayed compared with the right radial pulse. The blood pressure in the lower extremities is lower than that in the upper extremities. If cardiac function is poor, however, these differences may not be as apparent until appropriate resuscitation is accomplished. Decreased or absent lower extremity pulses, hypertension (upper extremity), or a murmur may be present. If significant collaterals have developed, continuous murmurs may be heard throughout the chest.
Seizures may be associated with abnormal eye movements treatment variable buy pirfenex 200mg line, such as tonic deviation to one side symptoms of depression 200mg pirfenex free shipping. The electroencephalogram often shows seizure activity when the clinical diagnosis is uncertain. Identifying seizures in the newborn period is often difficult because the infant, especially the low birth weight infant, usually does not show the tonic-clonic major motor activity typical of the older child (Table 64-1). The subtle signs of seizure activity include apnea, eye deviation, tongue thrusting, eye blinking, fluctuation of vital signs, and staring. Continuous bedside electroencephalographic monitoring can help identify subtle seizures. The diagnostic evaluation of infants with seizures should involve an immediate determination of capillary blood glucose levels with a Chemstrip. In addition, blood concentrations of sodium, calcium, glucose, and bilirubin should be determined. When infection is suspected, cerebrospinal fluid and blood specimens should be obtained for culture. After the seizure has stopped, a careful examination should be done to identify signs of increased intracranial pressure, congenital malformations, and systemic illness. If signs of 226 Section 11 u Fetal and Neonatal Medicine and hemorrhage because of passive changes in cerebral blood flow occurring with the variations of blood pressure that sick premature infants often exhibit (failure of autoregulation). In some sick infants, these blood pressure variations are the only identifiable etiologic factors. Many infants with small hemorrhages (grade 1 or 2) are asymptomatic; infants with larger hemorrhages (grade 4) often have a catastrophic event that rapidly progresses to shock and coma. Grade 4 hemorrhage has a poor prognosis, as does the development of periventricular, small, echolucent cystic lesions, with or without porencephalic cysts and posthemorrhagic hydrocephalus. Periventricular cysts often are noted after the resolution of echodense areas in the periventricular white matter. The cysts may correspond to the development of periventricular leukomalacia, which may be a precursor to cerebral palsy. They are associated with a high mortality rate and have a poor neurodevelopmental prognosis for survivors. Treatment of an acute hemorrhage involves standard supportive care, including ventilation for apnea and blood transfusion for hemorrhagic shock. Posthemorrhagic hydrocephalus may be managed with serial daily lumbar punctures, an external ventriculostomy tube, or a permanent ventricular-peritoneal shunt. Implementation of the shunt often is delayed because of the high protein content of the hemorrhagic ventricular fluid. If the diagnosis is not apparent at this point, further evaluation should involve magnetic resonance imaging, computed tomography, or cerebral ultrasound and tests to determine the presence of an inborn error of metabolism. Determinations of inborn errors of metabolism are especially important in infants with unexplained lethargy, coma, acidosis, ketonuria, or respiratory alkalosis. The treatment of neonatal seizures may be specific, such as treatment of meningitis or the correction of hypoglycemia, hypocalcemia, hypomagnesemia, hyponatremia, or vitamin B6 deficiency or dependency. In the absence of an identifiable cause, therapy should involve an anticonvulsant agent, such as 20 to 40 mg/kg of phenobarbital, 10 to 20 mg/kg of phenytoin, or 0. Treatment of status epilepticus requires repeated doses of phenobarbital and may require diazepam or midazolam, titrated to clinical signs. The long-term outcome for neonatal seizures usually is related to the underlying cause and to the primary pathology, such as hypoxic-ischemic encephalopathy, meningitis, drug withdrawal, stroke, or hemorrhage. Subdural hemorrhages are seen in association with birth trauma, cephalopelvic disproportion, forceps delivery, large for gestational age infants, skull fractures, and postnatal head trauma. Anemia, vomiting, seizures, and macrocephaly may occur in an infant who is 1 to 2 months of age and has a subdural hematoma. Child abuse in this situation should be suspected and appropriate diagnostic evaluation undertaken to identify other possible signs of skeletal, ocular, or soft tissue injury. Occasionally, a massive subdural hemorrhage in the neonatal period is caused by rupture of the vein of Galen or by an inherited coagulation disorder, such as hemophilia. Subarachnoid hemorrhages may be spontaneous, associated with hypoxia, or caused by bleeding from a cerebral arteriovenous malformation. Seizures are a common presenting manifestation, and the prognosis depends on the underlying injury.
It has an excellent safety profile due to a ceiling effect on respiratory suppression (meaning higher doses will not stop breathing and only rarely cause overdose) symptoms vertigo order pirfenex on line. Like any opioid medications post mi order discount pirfenex line, buprenorphine should be used sparingly, and only when the benefit outweighs the risk. Elderly Patients with Chronic Pain For elderly patients using long-term opioids, transitioning to buprenorphine lowers the risk of accidental overdose and potentially lowers the risk of medical complications. For this reason, buprenorphine may be a safer choice for elderly patients already on daily opioid treatment. As with all opioid analgesics, buprenorphine should be used sparingly for pain after both nonpharmacologic interventions and nonopioid analgesics have failed. Pharmacies should send the claim to fee-for-service Medi-Cal, not the managed Medi-Cal plan, as all buprenorphine products are carved out from managed care. Prescribers should write a justification on the script about why other covered drugs are not appropriate. Hospitalized and Perioperative Patients on Buprenorphine Discontinuing methadone or buprenorphine in the hospital puts patients at risk for pain exacerbation, return to use, and longer lengths of stay; in addition, patients face logistical challenges starting back on buprenorphine after discontinuation. The patient cap can increase to 275 patients for physicians board-certified in addiction, or those in practices that meet certain qualifications: 24-hour call coverage, California Health Care Foundation The "three-day rule" also allows buprenorphine administration (not prescription) by any licensed provider in any setting for up to three days while a patient is transitioning into ongoing treatment. Commercial insurance plans have different rules about buprenorphine coverage for pain and addiction and may require the prescriber to contact the plan or submit an authorization form. Informed consent and treatment agreements are often used in practice, but they have not been studied and should not be implemented in a way that increases barriers to treatment. The applicability of these rules varies depending on the type of provider, whether the provider "holds themselves out" as a substance use treatment provider, and the sources of funding. When prescribed for pain, it is helpful to write the pain diagnosis and justification on the script as well. Prescribers should confirm that their local pharmacy stocks buprenorphine and that, in states where substance use disorder treatment is carved out of managed care, the pharmacist knows the procedure for billing Medicaid. Pharmacies can be partners in addiction treatment by working with prescribing doctors to dispense small supplies of buprenorphine for high-risk patients and by alerting the prescriber when the patient is having difficulty, such as sedation. About the Foundation the California Health Care Foundation is dedicated to advancing meaningful, measurable improvements in the way the health care delivery system provides care to the people of California, particularly those with low incomes and those whose needs are not well served by the status quo. We work to ensure that people have access to the care they need, when they need it, at a price they can afford. For more information, see "Transdermal Buprenorphine, Opioid Rotation to Sublingual Buprenorphine, and the Avoidance of Precipitated Withdrawal: A Review of the Literature and Demonstration in Three Chronic Pain Patients Treated with Butrans," the Use of Transdermal Buprenorphine Patches in Aiding in Opioid Withdrawal: Clinical Effectiveness and Guidelines and "Transdermal Buprenorphine to Switch Patients from Higher Dose Methadone to Buprenorphine Without Severe Withdrawal Symptoms. Replace half of methadone with long-acting opioid for 3 to 4 days, then replace the other half for 3 to 4 days. Replace one-quarter to one-half of methadone with long-acting opioid for 3 to 4 days and repeat in two to four steps. Prescribe the following medications: $$ Buprenorphine Background With changing prescribing practices, many patients taking high-dose opioids for years are being tapered to lower doses or off opioids altogether. However, people with long-term opioid use for pain develop the same neurochemical changes seen in addiction, and opioid discontinuation is poorly tolerated, especially when done abruptly. Using buprenorphine patches during induction can ease the symptoms of withdrawal during the transition. The information is intended to serve as a guideline, not a replacement for individual medical judgment. The buprenorphine mono product (without naloxone) is less expensive than the combination product, with similar efficacy; either can be used. Note: Home starts on sublingual buprenorphine are appropriate for stable patients with good support, when the office can be contacted for questions; otherwise, the first sublingual buprenorphine doses should be observed in the office. After 3 to 4 days, instruct the patient to take the last short-acting opioid dose at night and start 1 mg (half-tablet) in the morning.
Generic pirfenex 200mg otc. Flu-like symptoms hammering local hospitals.
Syndromes
- Fetal monitoring
- Nonprescription medications that you might need
- Joint swelling with warm, tender joints
- Abdominal and pelvic adhesions can cause chronic pain.
- Fever
- Urinalysis
- Growths in or around the uterus and ovaries (such as cysts or fibroids)
- Immunodiffusion test
Immediately before term 5 medications order 200mg pirfenex visa, the infant begins to synthesize beta-hemoglobin chains; the term infant should have some adult hemoglobin (two alpha chains and two beta chains) symptoms 37 weeks pregnant 200 mg pirfenex. For a term infant, blood volume is 72 to 93 mL/kg, and for a preterm infant, blood volume is 90 to 100 mL/kg. The placenta and umbilical vessels contain approximately 20 to 30 mL/kg Gastrointestinal Bleeding Anemia Bleeding Petechiae/Purpura Pancytopenia Symptomatic anemia in the newborn period. Decreased Red Blood Cell Production Increased Red Blood Cell Destruction Immunologically mediated hemolysis in utero may lead to erythroblastosis fetalis, or the fetus may be spared and hemolytic disease may appear in the newborn. Hemolysis of fetal erythrocytes is a result of blood group differences between the sensitized mother and fetus, which causes production of maternal IgG antibodies directed against an antigen on fetal cells. These IgG antibodies cross the placenta by active transport and affect the fetus or newborn. The physician obtains information from the family, maternal and labor and deliv- maternal circulation, such as first-trimester abortion, ectopic pregnancy, amniocentesis, manual extraction of the placenta, version (external or internal) procedures, or normal pregnancy. It may produce hemolytic disease of the newborn, which is manifested as significant anemia and hyperbilirubinemia. Because many mothers who have blood group O have IgG antibodies to A and B before pregnancy, the firstborn infant of A or B blood type may be affected. Most Rh-negative women have no anti-Rh antibodies at the time of their first pregnancy. The Rh antigen system consists of five antigens: C, D, E, c, and e; the d type is not antigenic. In most Rh-sensitized cases, the D antigen of the fetus sensitizes the Rh-negative (d) mother, resulting in IgG antibody production during the first pregnancy. Because most mothers are not sensitized to Rh antigens at the start of pregnancy, Rh erythroblastosis fetalis is usually a disease of the second and subsequent pregnancies. The first affected pregnancy results in an antibody response in the mother, which may be detected during antenatal screening with the Coombs test and determined to be anti-D antibody. The first affected newborn may show no serious fetal disease and may manifest hemolytic disease of the newborn only by the development of anemia and hyperbilirubinemia. Subsequent pregnancies result in an increasing severity of response because of an earlier onset of hemolysis in utero. Fetal anemia, heart failure, elevated venous pressure, portal vein obstruction, and hypoalbuminemia result in fetal hydrops, which is characterized by ascites, pleural and pericardial effusions, and anasarca (see Chapter 60). The management of a pregnancy complicated by Rh sensitization depends on the severity of hemolysis, its effects on the fetus, and the maturity of the fetus at the time it becomes affected. The severity of the hemolysis can be assessed by the quantity of bilirubin transferred from the fetus to the amniotic fluid, quantified by spectrophotometric analysis of the optical density (at 450 nm) of amniotic fluid. The hemoglobin content and serum iron levels initially are normal, but the hemoglobin levels decline during the subsequent 24 hours. Newborns with chronic blood loss caused by chronic fetal-maternal hemorrhage or a twin-totwin transfusion present with marked pallor, heart failure, hepatosplenomegaly with or without hydrops, a low hemoglobin level at birth, a hypochromic microcytic blood smear, and decreased serum iron stores. Fetal-maternal bleeding occurs in 50% to 75% of all pregnancies, with fetal blood losses ranging from 1 to 50 mL; most blood losses are 1 mL or less, 1 in 400 are approximately 30 mL, and 1 in 2000 are approximately 100 mL. The diagnosis of fetal-maternal hemorrhage is confirmed by the Kleihauer-Betke acid elution test. Three zones of optical densities with decreasing slopes toward term gestation have been developed to predict the severity of the illness. If the lungs are immature and the fetus is between 22 and 33 weeks of gestational age, an ultrasound-guided intrauterine transfusion with O-negative blood into the umbilical vein is indicated and may have to be repeated until pulmonary maturity is reached or fetal distress is detected. Indications for fetal intravascular transfusion in sensitized fetuses between 22 and 32 weeks of gestational age include a fetal hematocrit of less than 25% to 30%, fetal hydrops, and fetal distress too early in gestation for delivery. Intravascular intrauterine transfusion corrects fetal anemia, improves the outcome of severe hydrops, and reduces the need for postnatal exchange transfusion, but is associated with neonatal anemia as a result of continued hemolysis plus suppressed erythropoiesis. Other blood group antigens that can cause immune hydrops and erythroblastosis include Rh C, E, Kell, and Duffy.

