Allegra
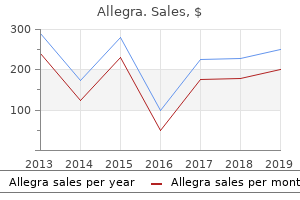
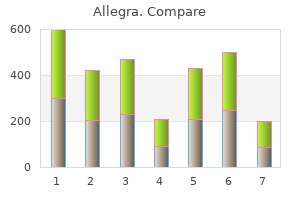
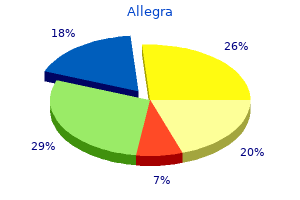
"Cost of allegra, allergy x capsules".
By: S. Yasmin, M.A., M.D., Ph.D.
Clinical Director, University of California, Davis School of Medicine
His renal function is normal allergy medicine like singulair order allegra pills in toronto, so digoxin renal clearance should not be significantly altered allergy medicine yeast infection discount 180 mg allegra visa. It has been observed that twice as much digitalis is required to produce toxicity in patients with serum potassium of 5 mEq/L than in those with a serum potassium of 3 mEq/L. Therefore, drugs, diseases, and medical maneuvers that induce hypokalemia or reduce the serum potassium from elevated to normal levels may unmask digitalis toxicity. A low serum potassium has been observed to increase the uptake of digitalis by the myocardial tissue. All diuretics, with the exception of potassium-sparing diuretics, can cause hypokalemia through kaliuresis. In addition, prednisone in high doses promotes potassium excretion in the distal portion of the renal tubule. Similarly, hypokalemia can result from diarrheal losses, including drug-induced diarrhea. Although the relationship of hypokalemia to digitalis toxicity is stressed, hyperkalemia is also a risk factor. Alkalosis results in the redistribution of potassium intracellularly and an increased renal excretion of potassium, thereby potentiating effects of hypokalemia (see Chapter 10, Acid-Base Disorders). In addition, alkalosis in and of itself has been associated with an increased incidence of digitalis toxicity. This is attributed to an intracellular depletion of potassium caused by increased urinary excretion and a relative increase in the ratio of extracellular to intracellular potassium. The causes are the same as for hypokalemia, including diuretic therapy, nasogastric suction losses, and chronic alcoholism. The prevalence of hypomagnesemia is higher in digitalis-toxic patients; magnesium sulfate has been used successfully in the treatment of digitalis toxicity. The electrical and contractile effects of calcium on the myocardium are similar to those of digitalis. The clinical significance of calciuminduced digitalis toxicity is questionable; there have been no reports of digitalis toxicity secondary to oral administration of calcium-containing products. Age may be an important predisposing factor in the production of digitalis toxicity in B. It is important to emphasize that, although the serum creatinine of elderly patients may be within normal limits, the mean creatinine clearance is reduced. The response to digitalis also can be altered in the very young (see Question 45). Lower doses are recommended in premature infants and neonates (<1 month) because of the decreased renal function normally observed in newborns. Withholding Digitalis and Electrolyte Replacement For many patients without life-threatening arrhythmias or major electrolyte imbalances, simple withdrawal of digitalis is the only treatment required. Although it may take five half-lives for the drug to be totally eliminated from the body, the serum concentration will drop to a safe level after one to two half-lives (2 to 3 days for digoxin) in most individuals. As a general rule, potassium replacement should be considered in any patient with digitalis-induced ectopic beats who has low or normal serum potassium levels. Oral administration is acceptable unless the patient cannot take medication orally or has life-threatening ectopy. If digitalis-induced arrhythmias are sufficiently severe to warrant intravenously administered potassium, the maximal recommended rate of administration is 40 mEq/hour (preferably 10 mEq/hour) at a concentration not exceeding 80 to 100 mEq/L. A total of several hundred milliequivalents of potassium might be required to replete body stores. It is important to obtain a serum magnesium concentration when measuring potassium levels. The infusion should be discontinued if deep tendon reflexes are diminished or serum concentrations of magnesium exceed 7 mEq/L. Atropine should be used with caution in patients with prostatic hypertrophy because significant urinary retention and postrenal azotemia can occur. Virtually all of the antiarrhythmic agents have been used to treat digitalis-induced arrhythmias.
Thioridazine is recognized as the most common cause of antipsychotic-induced sexual dysfunction allergy easy order 120mg allegra visa. Lowering the dose of thioridazine or converting him to another antipsychotic with less influence on sexual function may be helpful allergy forecast in michigan cheap allegra 120mg amex, although no reliable evidence is available to indicate which drugs are least likely to cause sexual dysfunction. In instances in which symptoms improve after the dose is increased, it may be difficult to know whether the response resulted from the dose change or from additional days on the drug. The duration of a therapeutic trial is 3 to 8 weeks in patients with little to no response, and 5 to 12 weeks in patients with a partial response. Antipsychotic drugs can lower the seizure threshold, producing seizures in patients who previously were seizure free. Strategies to minimize the risk of seizures should be employed and include slow dose titration, use of lowest effective doses, and possible concurrent administration of an antiepileptic drug. The decision to use scheduled or as-needed medications should be based on whether she remains dangerous after a few immediate doses and the underlying cause of the psychosis. Carbamazepine (and other enzyme-inducing antiepileptic drugs) can influence the hepatic metabolism of antipsychotic agents. Factors to Consider When Evaluating a Poor Response A large proportion of patients with schizophrenia do not have an adequate response to antipsychotic therapy. Inadequate response may be caused by inadequate dosing, poor adherence, or true resistance to antipsychotic treatment. In some patients, the therapeutic antipsychotic dose cannot be reached because of intolerable side effects. As mentioned, a therapeutic trial of 3 to 12 weeks at an optimal dosage may be necessary to determine the full benefit from an antipsychotic agent. Nonadherence with medications is a common obstacle in the management of schizophrenia, even in supervised settings. Blood level monitoring may be helpful to identify nonadherent patients as well as those in whom a pharmacokinetic factor may account for a poor response. A single definition of treatment resistance does not exist, but factors to consider in this definition include chronic or repeated hospitalizations, persistent positive symptoms, lack of improvement in negative symptoms, and breakthrough symptoms despite adherence to treatment. None of these strategies has been demonstrated to be superior to another in terms of efficacy or safety, and the switch strategy depends on the clinical presentation. If higher oral doses are needed for stabilization, then the first decanoate dose should be 15 to 20 times the oral daily dose to a maximum of 450 mg. Because haloperidol accumulates, the monthly decanoate dose should be decreased every 3 to 4 months by 25% until a minimum effective dose is achieved. Most patients can be effectively managed with a maintenance dose of 50 to 200 mg every 4 weeks. A 200-mg total dose is also acceptable if the clinician believes the patient needs more drug. No oral medication is needed after the second injection and should only be given if M. He should be able to tolerate higher potency antipsychotics because he has tolerated moderate doses of thiothixene. The patient should also be asked whether he is willing to take injections before proceeding with this strategy. The trial is necessary to ensure tolerability, evaluate response, and, when possible, determine the minimum effective dose. Various formulas to convert from oral formulations to the decanoates have been proposed, but no method has been proved clinically superior. Clinicians should strive to use the longest dosing interval between injections and minimize the duration of combination oral and depot therapy. He repeatedly presents in a paranoid and hostile state complaining of auditory hallucinations and paranoid delusions in which the police and the people in his apartment building are trying to kill him. His symptoms have prevented him from obtaining employment, and he has no close friends. In a double-blind trial comparing risperidone with haloperidol in treatment-refractory schizophrenia, a significantly higher response rate favoring risperidone was observed at week 4 but not at week 8.
What methods of insulin administration are available to achieve optimal glucose control A physiological insulin regimen is designed to mimic normal insulin secretion as closely as possible allergy guidelines 2015 allegra 180mg low cost. Before the development of the rapidacting insulin analogs and basal insulins allergy symptoms glands swollen discount 120mg allegra with mastercard, previous insulins lacked pharmacodynamic profiles that allowed one to closely simulate the basal-bolus model (see text that follows). In the nondiabetic individual, the pancreas secretes boluses of insulin in response to snacks and meals. Between meals and throughout the night, the pancreas secretes small amounts of insulin that are sufficient to suppress lipolysis and hepatic glucose output (basal insulin). Two methods have been used to achieve a similar pattern of insulin release: (a) insulin pump therapy (previously referred to as "continuous subcutaneous infusion of insulin") and (b) basal-bolus insulin regimens consisting of once to twice daily doses of basal insulin coupled with pre-meal doses of rapid or short-acting insulin (see Question 6). Insulin Pump Therapy the use of an insulin pump is currently the most precise way to mimic normal insulin secretion. This consists of a batteryoperated pump and a computer that can program the pump to deliver predetermined amounts of regular insulin, insulin lispro, insulin aspart, or insulin glulisine from a reservoir to a subcutaneously inserted catheter or needle. A bolus of regular insulin can be released by the patient 30 minutes before food ingestion. Most patients using an insulin pump, however, prefer to use the rapid-acting insulin analogs in their pump. For meal coverage, the rapid-acting insulin can be given 0 to 15 minutes before eating. The preferred meal planning approach for patients using an insulin pump is carbohydrate counting. The "insulin to carbohydrate ratio" or how much carbohydrate is covered by 1 unit of insulin must be determined. Many patients find it advantageous to decrease the basal rate during the middle of the night when nocturnal hypoglycemia is most likely to occur. The basal rate also may be increased before awakening to avoid hyperglycemia secondary to the "dawn phenomenon"-adjustments that are not possible using subcutaneous basal insulin injections. Features of the current pump models include "bolus wizard," which calculates accurate boluses based on preset carbohydrate-to-insulin ratios and correction factors, carbohydrate counts for selected foods, and an "insulin-on-board" feature, which avoids stacking of insulin doses by indicating how much insulin from a previously administered dose is still available. Most insurance plans provide coverage for insulin pumps for patients with type 1 and some patients with type 2 diabetes. Factors to consider when choosing a pump include safety features, durability, ability of the manufacturer to provide service, availability of training, clinically desirable features, and cosmetic attractiveness for the user. Endocrinologists have developed a variety of insulin regimens that are intended to mimic the release of insulin from the pancreas. A regimen much less commonly used in patients with type 1 diabetes involves injecting a mixture of intermediate-acting and regular or rapid-acting insulin twice daily, before breakfast and before dinner. B: Morning injection of rapid or short-acting insulin and an intermediate-acting insulin, a presupper injection of rapid or short-acting insulin, and a bedtime injection of intermediate-acting insulin. Suggested for patients with early morning hypoglycemia followed by rebound hyperglycemia or for patients with early morning hyperglycemia (rebound phenomenon). Arrows, time of insulin injection (<15 minutes before meals for rapid-acting insulin and 30 minutes before meals for short-acting insulin). This shifts the time of peak effect from approximately 2 to 3 am to approximately 7 am. This method may be useful for patients in whom nocturnal hypoglycemia and fasting hyperglycemia are particularly troublesome; however, this regimen also does not mimic physiological insulin release. The regimen that most closely mimics physiological insulin release besides the use of an insulin pump, is the use of a once-daily basal insulin such as insulin glargine or insulin detemir to provide basal insulin levels throughout the day, along with doses of regular, insulin lispro, insulin aspart or insulin glulisine before meals. When smaller doses are used, twice-daily insulin detemir and possibly insulin glargine will be required for 24-hour coverage. For example, if a patient with diabetes chooses to skip a meal, he or she omits a premeal bolus; if the patient chooses to eat a larger meal than usual, he or she increases the premeal bolus. Similar dose adjustments can be made to accommodate snacks, exercise patterns, and acute illnesses.
Comparison of ofloxacin and ceftriaxone for short-course treatment of enteric fever allergy symptoms upper respiratory allegra 180 mg free shipping. Two or three days of ofloxacin treatment for uncomplicated multidrug-resistant typhoid fever in children allergy symptoms rhinitis buy line allegra. Azithromycin versus ciprofloxacin for treatment of uncomplicated typhoid fever in a randomized trial in Egypt that included patients with multidrug resistance. Randomized controlled comparison of ofloxacin, azithromycin, and an ofloxacin-azithromycin combination for treatment of multidrug-resistant and nalidixic acid-resistant typhoid fever. Azithromycin versus ceftriaxone for the treatment of uncomplicated typhoid fever in children. Failure of short-course ceftriaxone chemotherapy for multidrug-resistant typhoid fever in children: a randomized controlled trial in Pakistan. Quinolone-resistant Salmonella typhi in Vietnam: molecular basis of resistance and clinical response to treatment. A comparative study of ofloxacin and cefixime for treatment of typhoid fever in children. Reduction of mortality in chloramphenicol-treated severe typhoid fever by high-dose dexamethasone. Treatment of chronic carriers of Salmonella typhi and Salmonella paratyphi with trimethoprim-sulfamethoxazole. The central Scotland Escherichia coli O157:H7 outbreak: risk factors for the hemolytic uremic syndrome and death among hospitalized patients. Shiga toxin-producing Escherichia coli in children with diarrhea: a prospective pointof-care study. The United States National Prospective Hemolytic Uremic Syndrome Study: microbiologic, serologic, clinical, and epidemiologic findings. A classification of hemolytic uremic syndrome and thrombotic thrombocytopenic purpura and related disorders. Predictors for the development of haemolytic uraemic syndrome with Escherichia coli O157:H7 infections: with focus on the day of illness. Risk factors for the progression of Escherichia coli O157:H7 enteritis to hemolyticuremic syndrome. A nationwide case-control study of Escherichia coli O157:H7 infection in the United States. A severe outbreak of Escherichia coli O157:H7-associated hemorrhagic colitis in a nursing home. Randomized, controlled trial of antibiotic therapy for Escherichia coli O157:H7 enteritis. Hemolytic-uremic syndrome during an outbreak of Escherichia coli O157:H7 infections in institutions from mentally retarded persons: clinical and epidemiologic observations. Risk of hemolytic uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 enteritis: a meta-analysis. Systematic review: are antibiotics detrimental or beneficial for the treatment of patients with Escherichia coli O157:H7 infection Prediction of hemolytic uremic syndrome in children during a large outbreak of Escherichia coli O157:H7 infections. Safety and immunogenicity of Escherichia coli O157 O-specific polysaccharide conjugate vaccine in 2-5-year-old children. Transmission of Escherichia coli O157:H7 infection in Minnesota child day-care facilities. A meta-analysis on the effects of antibiotic treatment on duration of symptoms caused by infection with campylobacter species. Adverse health events associated with antimicrobial drug resistance in campylobacter species: a registry-based cohort study. Double-blind placebo-controlled study of erythromycin for treatment of Campylobacter enteritis. Use of azithromycin for the treatment of Campylobacter enteritis in travelers to Thailand, an area where ciprofloxacin resistance is prevalent. Azithromycin found to be comparable to levofloxacin for the treatment of us travelers with acute diarrhea acquired in Mexico. Occurrence and self-treatment of diarrhea in a large cohort of Americans traveling to r 62-25 99. Interactions of fluoroquinolones with other drugs: mechanisms, variability, clinical significance, and management.
Available binders include products that contain calcium allergy medicine rx allegra 120 mg on-line, lanthanum allergy shots over the counter purchase allegra 120mg mastercard, aluminum, or magnesium cations or the polymer-based agent, sevelamer hydrochloride (Renagel). Correction of hypocalcemia is an added beneficial effect of the calcium-containing preparations; however, a risk exists of hypercalcemia and cardiac calcification associated with the prolonged use of these agents. Although calcium-containing binders have an added benefit of correcting hypocalcemia, the potential for hypercalcemia must be frequently evaluated in patients receiving these agents chronically. Simultaneous administration of vitamin D preparations and calcium also increases the risk of hypercalcemia. A "corrected" serum calcium and the "Ca-P product" (defined below) should be determined before therapy is started and at regular intervals thereafter. Calculating corrected calcium adjusts for the change in the ratio of free (unbound) versus protein bound calcium owing to reduced serum albumin concentrations. Based on the increased risk of mortality associated with an elevated Ca-P product and the potential for cardiac calcification, the ideal Ca-P product target has been decreased to <55 mg2 /dL2. When the Ca-P product exceeds the target value, the patient should be switched to a noncalcium-based phosphate binder. Alternatives include sevelamer and cations, such as lanthanum carbonate, aluminum, or magnesium preparations. For patients requiring dialysis, reducing the calcium concentration of the dialysate bath may decrease the risk of hypercalcemia. Nausea, diarrhea, and constipation are other side effects of calcium-containing products. Because calcium-containing binders may interact with other drugs, timing of their administration relative to other agents must be considered. Fluoroquinolones and oral iron, for example, should be taken at least 1 or 2 hours before calcium-containing phosphate binders. Importantly, if the calcium products are being used as supplementation to treat hypocalcemia or osteoporosis, they should be taken between meals to enhance intestinal absorption. This is in contrast to their administration with meals if they are being used as phosphate binders. Starting doses of common calciumcontaining phosphate binders are listed in Table 31-7. Dosing guidelines for sevelamer are also available for patients being converted from calcium acetate. Based on studies showing similar reductions in serum phosphorus, 800 mg of sevelamer is considered equivalent to 667 mg of calcium acetate (169 mg elemental calcium). Several studies have confirmed this effect and it should be taken into account when using this agent. When ingested, it dissociates into a trivalent cation with similar binding capacity as aluminum salts, and lanthanum also has been found to be as effective and tolerable as standard treatment. Studies have evaluated the deposition and toxicity of lanthanum in the bone, liver, and brain because of concerns of lanthanum accumulation. The recommended initial total daily dose is 750 to 1,500 mg given with meals and dosage titration up to a maximal dosage of 3,000 mg daily should be based on serum phosphate levels. The most frequent adverse events reported in clinical trials are nausea and vomiting. Elevated serum aluminum concentrations and aluminum deposition in bone and other tissues of patients with kidney disease have been associated with osteomalacia, microcytic anemia, and a fatal neurologic syndrome, referred to as dialysis encephalopathy. Aluminum-containing agents should only be considered on a short-term basis (up to 4 weeks) for patients with an elevated Ca-P product; however, sevelamer is generally preferred in these situations. Sucralfate, used primarily for the treatment of ulcers, also contains aluminum and should be used cautiously in patients with kidney disease. Magnesium agents (magnesium hydroxide, magnesium carbonate) may be beneficial, but as with aluminum, their use should be limited, because at the high doses required to control serum phosphorus concentrations, severe diarrhea and hypermagnesemia invariably result. Magnesium might, however, be considered in patients whose serum phosphorus concentrations cannot be controlled adequately by other phosphatebinding agents.
Buy allegra once a day. Allergic rhinitis/homeopathy medicine for allergic rhinitis/homeopathic medicine for sneezing.