Thyroxine
"Generic thyroxine 75mcg free shipping, medicine lake california".
By: Z. Snorre, M.B.A., M.B.B.S., M.H.S.
Deputy Director, Kaiser Permanente School of Medicine
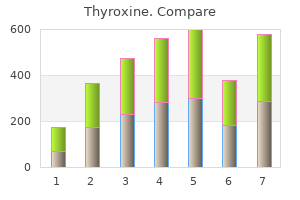
Central Cord Syndrome Central cord syndrome is most often caused by hyperextension of the cervical region of the spine medicine quinidine order thyroxine with american express. The cord is pressed on anteriorly by the vertebral bodies and posteriorly by the bulging of the ligamentum flavum medicine dictionary purchase discount thyroxine on-line, causing damage to the central region of the spinal cord. Radiographs of these injuries often appear normal because no fracture or dislocation has occurred. The following characteristic clinical features are seen after the period of spinal shock has ended: 1. Bilateral spastic paralysis below the level of the lesion with characteristic sacral "sparing. Bilateral loss of pain, temperature, light touch, and pressure sensations below the level of the lesion with characteristic sacral "sparing. It follows from this discussion that the clinical picture of a patient with a history of a hyperextension injury of the neck, presenting with motor and sensory tract injuries involving principally the upper limb,would strongly suggest central cord syndrome. The sparing of the lower part of the body may be evidenced by (1) the presence of perianal sensation, (2) good anal sphincter tone, and (3) the ability to move the toes Destructive Spinal Cord Syndromes When neurologic impairment is identified following the disappearance of spinal shock, it can often be categorized into one of the following syndromes: (1) complete cord transection syndrome, (2) anterior cord syndrome, (3) central cord syndrome, or (4) Brown-Sйquard syndrome or hemisection of the cord. The clinical findings often indicate a combination of lower motor neuron injury (at the level of destruction of the cord) and upper motor neuron injury (for those segments below the level of destruction). It can be caused by fracture dislocation of the vertebral column, by a bullet or stab wound, or by an expanding tumor. The following characteristic clinical features will be seen after the period of spinal shock has ended: 1. Bilateral lower motor neuron paralysis and muscular atrophy in the segment of the lesion. A bilateral Babinski sign is present,and depending on the level of the segment of the spinal cord damaged, bilateral loss of the superficial abdominal and cremaster reflexes occurs. All these signs are caused by an interruption of the corticospinal tracts on both sides of the cord. The bilateral spastic paralysis is produced by the cutting of the descending tracts other than the corticospinal tracts. The loss of tactile discrimination and vibratory and proprioceptive sensations is due to bilateral destruction of the ascending tracts in the posterior white columns. The loss of pain, temperature, and light touch sensations is caused by section of the lateral and anterior spinothalamic tracts on both sides. Because these tracts cross obliquely, the loss of thermal and light touch sensations occurs two or three segments below the lesion distally. Bladder and bowel functions are no longer under voluntary control, since all the descending autonomic fibers have been destroyed. Clinical Notes 171 Complete cord transection syndrome Anterior cord syndrome Central cord syndrome Brown-Sequard syndrome Syringomyelia Poliomyelitis Amyotrophic lateral sclerosis Figure 4-31 Spinal cord syndromes. Brown-Sйquard Syndrome or Hemisection of the Cord Hemisection of the spinal cord can be caused by fracture dislocation of the vertebral column, by a bullet or stab wound, or by an expanding tumor. In patients whose damage is caused by edema of the spinal cord alone, the prognosis is often very good. A mild central cord syndrome that consists only of paresthesias of the upper part of the arm and some mild arm and hand weakness can occur. Ipsilateral lower motor neuron paralysis in the segment of the lesion and muscular atrophy. These signs are caused by damage to the neurons on the anterior gray column and possibly by damage to the nerve roots of the same segment. An ipsilateral Babinski sign is present, and depending on the segment of the cord damaged, an ipsilateral loss of the superficial abdominal reflexes and cremasteric reflex occurs. All these signs are due to loss of the corticospinal tracts on the side of the lesion. Spastic paralysis is produced by interruption of the descending tracts other than the corticospinal tracts. This results from the destruction of the posterior root and its entrance into the spinal cord at the level of the lesion. Ipsilateral loss of tactile discrimination and of vibratory and proprioceptive sensations below the level of the lesion.
Nodes of Ranvier are present in myelinated nerve fibers in the central nervous system symptoms 5th week of pregnancy buy 200mcg thyroxine. The major dense line of myelin consists of two inner protein layers of the plasma membrane that are fused together symptoms 7 cheap 200mcg thyroxine mastercard. The incisures of Schmidt-Lanterman represent where the dark major dense line is not formed as a result of the localized persistence of Schwann cell cytoplasm. As many as 15 or more unmyelinated axons may share a single Schwann cell in the peripheral nervous system. Chromatolysis is the term used to describe the changes in the arrangement of Nissl material within the cytoplasm of the nerve cell body following injury (see p. A single oligodendrocyte may be associated with the myelin sheaths of as many as 60 axons (see p. A single oligodendrocyte may be associated with several segments of myelin on a single axon. The incisures of Schmidt-Lanterman are present in the myelinated fibers of the central nervous system. Myelination in the central nervous system occurs by the growth in length of the oligodendrocytic process and the wrapping of it around the axon. A nonmyelinated axon in the central nervous system has no special relationship with the oligodendrocyte (see p. Spinal nerves are formed by the union of anterior and posterior nerve roots. The posterior root ganglion of a spinal nerve contains unipolar neurons enveloped in capsular cells. A peripheral nerve plexus situated at the root of a limb permits nerve fibers from different segments of the spinal cord to become rearranged so that they more easily travel to different parts of the limb (see p. In peripheral nerve plexuses, bundles of nerve fibers branch, but in most instances, the individual nerve fibers do not branch. The peripheral nerve plexuses at the roots of the limbs are formed from the anterior rami of the spinal nerves. The nerve plexuses of the autonomic nervous system possess a network of nerve fibers and nerve cells. In nerve conduction, an adequate stimulus increases the permeability of the axolemma to Na ions at the point of stimulation. During the absolute refractory period of nerve conduction, no stimulus, no matter how strong, will excite the nerve fiber. During nerve conduction, the action potential moves along the axon; the entry of Na ions into the axon ceases, and the permeability of the plasma membrane of the axon to K ions increases (see p. In the resting unstimulated nerve fiber, the interior of the plasma membrane (axolemma) is negative to the exterior. In nonmyelinated nerve fibers, the action potential occurs along the length of the fiber. The conduction velocity is greatest in nerve fibers having a large cross-sectional diameter. At the node of Ranvier, the action potential sets up an electrical current in the surrounding tissue fluid (see p. In wallerian degeneration, the myelin breaks down into droplets that are phagocytosed by the Schwann cells. In wallerian degeneration, the axon first breaks up into fragments before it is phagocytosed by the surrounding Schwann cells (see p. In wallerian degeneration, the Schwann cells proliferate rapidly and become arranged in parallel cords within the persistent basement membrane. In wallerian degeneration in the central nervous system, the debris is removed by the microglial cells. In wallerian degeneration in the peripheral nervous system, the tissue macrophages are very active in removing the nerve fragments. Following injury to the central nervous system, the oligodendrocytes fail to multiply and form a band fiber as do Schwann cells in the damaged peripheral nervous system (see p. The absence of endoneurial tubes may be important in the failure in the regeneration of injured central nervous system tissue (see p. The partial return of function seen in spinal cord injuries may be due in part to the patient using other muscles to compensate for the loss of the paralyzed muscles.
Buy thyroxine on line amex. Vlog#8: Opiate detox/withdrawal..
With further development medicine balls for sale discount thyroxine line, the axons of neurons forming these nuclei grow out into the mesencephalon (midbrain) to reach the forebrain symptoms 6 days after embryo transfer generic 75mcg thyroxine amex, and these fibers will form the greater part of the superior cerebellar peduncle. Later, the growth of the axons of the pontocerebellar fibers and the corticopontine fibers will connect the cerebral cortex with the cerebellum, and so the middle cerebellar peduncle will be formed. The inferior cerebellar peduncle will be formed largely by the growth of sensory axons from the spinal cord, the vestibular nuclei, and olivary nuclei. Midbrain (Mesencephalon) the midbrain develops from the midbrain vesicle,the cavity of which becomes much reduced to form the cerebral aqueduct or aqueduct of Sylvius. The sulcus limitans separates the alar plate from the basal plate on each side, as seen in the developing spinal cord. The neuroblasts in the basal plates will differentiate into the neurons forming the nuclei of the third and fourth cranial nerves and possibly the red nuclei, the substantia nigra, and the reticular formation. Also shown is the fusion of the rhombic lips in the midline to form the dumbbell-shaped cerebellum. The neuroblasts in the alar plates differentiate into the sensory neurons of the superior and inferior colliculi. Four swellings representing the four colliculi appear on the posterior surface of the midbrain. The superior colliculi are associated with visual reflexes, and the inferior colliculi are associated with auditory reflexes. With further development, the fibers of the fourth cranial nerve emerge on the posterior surface of the midbrain and decussate completely in the superior medullary velum. The fibers of the third cranial nerve emerge on the anterior surface between the cerebral peduncles. In the lateral wall of the third ventricle, the thalamus arises as a thickening of the alar plate on each side. Posterior to the thalamus, the medial and lateral geniculate bodies develop as solid buds. With the continued growth of the two thalami, the ventricular cavity becomes narrowed, and in some individuals,the two thalami may meet and fuse in the midline to form the interthalamic connection of gray matter that crosses the third ventricle. The lower part of the alar plate on each side will differentiate into a large number of hypothalamic nuclei. One of these becomes conspicuous on the inferior surface of the hypothalamus and forms a rounded swelling on each side of the midline called the mammillary body. The infundibulum develops as a diverticulum from the floor of the diencephalon, and from it will originate the stalk and pars nervosa of the hypophysis. The roof and floor plates remain thin, whereas the lateral walls become thick, as in the developing spinal cord. At an early stage, a lateral diverticulum called the optic vesicle appears on each side of the forebrain. That part of the forebrain that lies rostral to the optic vesicle is the telencephalon,and the remainder is the diencephalon. The telencephalon now develops a lateral diverticulum on each side of the cerebral hemisphere, and its cavity is known as the lateral ventricle. The anterior part of the third ventricle, therefore, is formed by the medial part of the telencephalon and ends at the lamina terminalis, which represents the rostral end of the neural tube. Fate of the Telencephalon the telencephalon forms the anterior end of the third ventricle, which is closed by the lamina terminalis, while the diverticulum on either side forms the cerebral hemisphere. Cerebral Hemispheres Each cerebral hemisphere arises at the beginning of the fifth week of development. As it expands superiorly, its walls thicken,and the interventricular foramen becomes reduced in size. The mesenchyme between each cerebral hemisphere condenses to form the falx cerebri. As development proceeds, the cerebral hemispheres grow and expand rapidly,first anteriorly to form the frontal lobes, then laterally and superiorly to form the parietal lobes, and finally posteriorly and inferiorly to produce the occipital and temporal lobes. As the result of this great expansion, the hemispheres cover the midbrain and hindbrain.
Treatment of volume contraction with the infusion of saline often corrects mild hypercalcemia medications kosher for passover order thyroxine 200 mcg with visa. Loop diuretics also increase calcium excretion treatment kidney failure order thyroxine on line, but diuretics may also facilitate nephrotoxicity from light chains and should be avoided, if possible. Glucocorticoid therapy (such as methylprednisolone) is helpful for acute management of the multiple myeloma as well as hypercalcemia. Bisphosphonates, such as pamidronate and zoledronic acid, are used to treat moderate hypercalcemia (serum calcium greater than 3. Bisphosphonates lower serum calcium by interfering with osteoclast-mediated bone resorption. Although hypercalcemia of myeloma responds to bisphosphonates, these agents can be nephrotoxic and should be administered only to euvolemic patients. Treatment with pamidronate or zoledronic acid allows outpatient management of mild hypercalcemia. In addition to controlling hypercalcemia, bisphosphonates appear to inhibit growth of plasma cells and have been used to treat multiple myeloma, particularly in patients with osseous lesions and bone pain. Kidney replacement therapy in the form of hemodialysis or peritoneal dialysis is generally recommended in patients with renal failure from monoclonal light-chain-related kidney diseases. Recovery of kidney function sufficient to survive without dialysis occurs in as many as 5% of patients with multiple myeloma, although in some patients this goal requires months to achieve, probably because the traditional chemotherapeutic regimens slowly reduce circulating lightchain levels. Despite the susceptibility to infection in multiple myeloma, the peritonitis rate for continuous ambulatory peritoneal dialysis (one episode every 14. Neither peritoneal dialysis nor hemodialysis appears to provide a superior survival advantage in patients with myeloma. Kidney transplant also has been performed successfully in selected patients with multiple myeloma in remission. Because the light chain is the underlying cause of cast nephropathy, tests that ensure absence of circulating free light chains are useful in the evaluation of candidacy for kidney transplantation. Kidney biopsy typically shows crystals of lightchain protein within the epithelium of the proximal tubule. Plasma cell dyscrasia should therefore be considered in the differential diagnosis when this syndrome occurs in adults. Unlike most endogenous low-molecular-weight proteins, monoclonal light chains have a propensity to produce tubular injury. Although the more common lesion is cast nephropathy, patients occasionally present with kidney failure from an isolated proximal tubulopathy that is distinct from the pathology associated with Fanconi syndrome. Kidney failure from isolated proximal tubular damage generally improves with effective chemotherapy that reduces the circulating monoclonal free light chain. A major mechanism of damage to the proximal epithelium is related to accumulation of toxic light chains in the endolysosome system. Loss of proximal tubular epithelial cells and generation of a proinflammatory milieu may also promote nephron dropout and the tubulointerstitial scarring and inflammation that are prevalent findings in cast nephropathy. The origin of these cells is thought to be a postantigenstimulated memory B cell that has undergone malignant transformation through somatic hypermutation. Lytic bone lesions are uncommon, but hepatosplenomegaly and lymphadenopathy are frequently identified. IgM is a large molecule that is not excreted and accumulates in the plasma to produce hyperviscosity syndrome, which consists of neurological symptoms (headaches, stupor, deafness, dizziness), visual impairment (from hemorrhages and edema), bleeding diathesis (related to IgM complexing clotting factors and to platelet dysfunction), kidney failure, and symptoms of hypervolemia. A reduced glomerular filtration rate occurs in about 30% of patients, and hyperviscosity syndrome and precipitation of IgM in the lumen of glomerular capillaries are the most common causes. Because of the typically advanced age at presentation (sixth to seventh decade) and slowly progressive course, the major therapeutic goal is relief of symptoms. All patients with IgM levels greater than 4 g/dl should have serum viscosity determined. Plasmapheresis is indicated in symptomatic patients and should be continued until symptoms resolve and serum viscosity normalizes. Factors that portend a worse outcome include age greater than 65 years and organomegaly. Recent advances in the understanding of pathophysiologic mechanisms underlying these disorders have distinguished them substantially from one another, with significant implications for clinical management.