Nizagara
"Buy nizagara 50mg fast delivery, erectile dysfunction and diabetes leaflet".
By: Z. Campa, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Medical Instructor, Florida State University College of Medicine
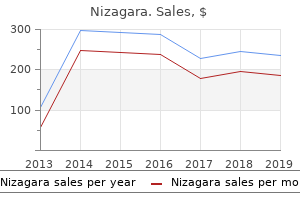
This is confusing as fetal presentations may change during pregnancy and it is not uncommon for twin B to be born first at cesarean section vasodilator drugs erectile dysfunction cheap nizagara 25mg line, which presents confusion for parents erectile dysfunction jet lag order nizagara master card. It is recommended to follow a descriptive process for twin labeling that takes into account the location of each gestational sac in relationship to maternal right or left side and the position of the sac in the uterus as upper or lower. When dichorionic twins are diagnosed in the first trimester, follow-up ultrasound is recommended at 18 to 20 weeks of gestation and if uncomplicated every 4 weeks thereafter. In one study, a combined risk assessment approach in the first and second trimester (16 weeks) ultrasound identified a subgroup of monochorionic twin pregnancies with a risk of complicated fetal outcome, reported as greater than 70% with a survival rate of only 69%. In monochorionic twins, Down syndrome risk is calculated as the average risk of both fetuses, whereas in dichorionic twins, the risk is calculated per fetus A and B. It is unclear whether the detection rate of Down syndrome is lower in twins than in singletons, as studies have shown conflicting results. The option for selective feticide should also be discussed with the patient during genetic counseling. The presence of twin discordance in fetal anomalies presents a challenging clinical scenario. In such cases, management at a center with expertise in fetal medicine is recommended. When one fetus of a dichorionic twin pregnancy presents with a lethal anomaly that carries a high risk for in utero demise, conservative management is generally recommended. These twins are discordant for anomaly as seen on three-dimensional ultrasound in surface mode. When ultrasound examinations are performed in the first trimester, about a third of twin pregnancies will ultimately result in singletons. As stated previously, biochemical markers for genetic screening are typically affected, especially when the vanishing twin occurs later in the first trimester. In this setting, careful attention should be given to ultrasound imaging with the application of color Doppler to rule out the presence of an acardiac twin with twin-reversed arterial perfusion (discussed later in this chapter). Follow-up ultrasound examinations in the second trimester are also important to rule out the presence of malformations in the surviving twin, especially involving the central nervous system. Of note, the earlier in gestation that the demise of a co-twin occurs in a monochorionic twin pregnancy, the lower is the risk of neurologic complication in the surviving twin member. In general, demise of a co-twin embryo/fetus in the first trimester in a dichorionic pregnancy typically results in a favorable outcome for the surviving twin member. The recipient twin fetus is typically plethoric, larger in size, and has polyhydramnios due to excess urination. The donor twin fetus is anemic, smaller in size, and has a "stuck" appearance due to oligohydramnios with restricted movements. In three-dimensional ultrasound in surface mode (C), fetuses (1) and (2) are seen, separated by a thick membrane (asterisk). In Europe, the diagnosis of polyhydramnios is made when the maximum vertical pocket is greater to or equal to 8 cm by 20 weeks of gestation and 10 cm after 20 weeks. The normal fetus perfuses the acardiac mass by an arterial-to-arterial anastomosis on the placental surface. Typically in normal conditions, the umbilical arteries carry blood from the fetus to the placenta. Given that the normal fetus has to perfuse his/her body and that of the acardiac mass, there is a significant increase in cardiac workload and a risk for cardiac failure and hydrops. The ratio of the estimated weight of the acardiac twin to that of the normal twin has been used to assess mortality risk. Bipolar cord coagulation of the acardiac twin appears to be the most feasible option for cord occlusion and is best performed before 24 weeks of gestation. Treatment intervention before 16 weeks of gestation is preferable when technically feasible. Note the presence of an amorphous mass of tissue with an amniotic membrane covering (small arrows) and a yolk sac, representing the acardiac twin. Often, a part of a spine (A) and some bones (A and B) are found and occasionally some parts of the lower body may be present along with lower extremities.
Diseases
- Glucose 6 phosphate dehydrogenase deficiency
- Amnesia, anterograde
- Macroglossia exomphalos gigantism
- Alar nasal cartilages coloboma of telecanthus
- Deletion 6q16 q21
- Chromosome 1, monosomy 1p32
- Progeria variant syndrome Ruvalcaba type
- Cataract congenital autosomal dominant
- Female pseudohermaphroditism
In the fully developed heart erectile dysfunction causes std buy 25 mg nizagara overnight delivery, the original embryonic left atrium is represented by little more than the trabeculated atrial appendage erectile dysfunction doctor visit buy discount nizagara 50 mg online, while the smooth-walled part originates from the pulmonary veins. On the right side, the original embryonic right atrium becomes the trabeculated right atrial appendage containing the pectinate muscles, and the smooth-walled sinus venarum originates from the right horn of the sinus venosus. Septum Formation in the Atrioventricular Canal At the end of the fourth week, two mesenchymal cushions, the atrioventricular endocardial cushions, appear at the anterior and posterior borders of the atrioventricular canal. Initially, the atrioventricular canal gives access only to the primitive left ventricle and is separated from the bulbus cordis by the bulbo (cono) ventricular flange. Near the end of the fifth week, however, the posterior extremity of the flange terminates almost midway along the base of the superior endocardial cushion and is much less prominent than before. Since the atrioventricular canal enlarges to the right, blood passing through the atrioventricular orifice now has direct access to the primitive left as well as the primitive right ventricle. In addition to the anterior and posterior endocardial cushions, the two lateral atrioventricular cushions appear on the right and left borders of the canal. The anterior and posterior cushions, in the meantime, project further into the lumen and fuse, resulting in a complete division of the canal into right and left atrioventricular orifices Interseptovalvular space Septum spurium Right venous valve Sinuatrial orifice Left venous valve Septum primum Pulmonary veins Superior vena cava Sinus venarum Septum secundum Septum primum Crista terminalis A B Figure 13. Both the wall of the right sinus horn (blue) and the pulmonary veins (red) are incorporated into the heart to form the smooth-walled parts of the atria. Common atrioventricular canal Superior endocardial cushion Right atrioventricular canal Lateral cushion Inferior endocardial cushion Left atrioventricular canal Figure 13. At this stage of development, blood from the atrial cavity enters the primitive left ventricle as well as the primitive right ventricle. Atrioventricular Valves After the atrioventricular endocardial cushions fuse, each atrioventricular orifice is surrounded by local proliferations of mesenchymal tissue. When the bloodstream hollows out and thins tissue on the ventricular surface of these proliferations, valves form and remain attached to the ventricular wall by muscular cords. Finally, muscular tissue in the cords degenerates and is replaced by dense connective tissue. They are connected to thick trabeculae in the wall of the ventricle, the papillary muscles, by means of chordae tendineae. In this manner, two valve leaflets, constituting the bicuspid (or mitral) valve, form in the left atrioventricular canal, and three, constituting the tricuspid valve, form on the right side. Dense mesenchymal tissue Lumen of ventricle Muscular chord Antrioventricular valves A Myocardium B C Papillary muscle Chordae tendineae Figure 13. The valves are hollowed out from the ventricular side but remain attached to the ventricular wall by the chordae tendineae. These ridges, the truncus swellings, or cushions, lie on the right superior wall (right superior truncus swelling) and on the left inferior wall (left inferior truncus swelling). The right superior truncus swelling grows distally and to the left, and the left inferior truncus swelling grows distally and to the right. Hence, while growing toward the aortic sac, the swellings twist around each other, foreshadowing the spiral course of the future septum. After complete fusion, the ridges form the aorticopulmonary septum, dividing the truncus into an aortic and a pulmonary channel. When the truncus swellings appear, similar swellings (cushions) develop along the right dorsal and left ventral walls of the conus cordis. The conus swellings grow toward each other and distally to unite with the truncus septum. When the two conus swellings have fused, the septum divides the conus into an anterolateral portion (the outflow tract of the right ventricle). Neural crest cells, originating in the edges of the neural folds in the hindbrain region, migrate through pharyngeal arches 3, 4, and 6 to the outflow region of the heart, which they invade. In this location, they contribute to endocardial cushion formation in both the conus cordis and truncus arteriosus. Therefore, outflow tract defects may Right conotruncal ridge Left conotruncal ridge Conotruncal septum Left atrioventricular orifice Right atrium Right atrioventricular orifice Proliferation of anterior atrioventricular cushion Muscular part of the interventricular septum Pulmonary channel A B Aortic channel Muscular part of the interventricular septum Membranous part of the interventricular septum C Figure 13. Proliferations of the right and left conus cushions, combined with proliferation of the anterior endocardial cushion, close the interventricular foramen and form the membranous portion of the interventricular septum. Septum secundum Right venous valve Oval foramen Right atrium Conus septum Septum primum Left atrium Outflow channel of left ventricle Outflow channel of right ventricle Right ventricle Muscular interventricular septum Left ventricle 7th week Figure 13. Chapter 13 Migrating neural crest cells Cardiovascular System 181 Septum Formation in the Ventricles By the end of the fourth week, the two primitive ventricles begin to expand.
Buy discount nizagara 100 mg online. Kill Erectile Dysfunction in 7 minutes || Get Harder And Longer Erections.
Bilious emesis is constant and the more proximal the obstacle impotence with diabetes effective nizagara 25 mg, the earlier and more abundant is the vomiting; the more distal the object erectile dysfunction treatment edmonton discount 100 mg nizagara overnight delivery, the greater the abdominal distension. With a distal obstruction, it is not always easy to di erentiate the small from the large bowel, and the obstructive site is di cult to evaluate because of the liquid content distal to it. As fetal screening indicates imaging immediately a er birth, the diagnostic e cacy of plain abdominal lms is reduced. Radiological data should therefore be complemented by neonatal ultrasound for diagnosis of small-bowel obstruction. On sonography, uid dilatation is seen up to the obstruction, and the loops of the thin-walled small bowel show increased hyperperistalsis. Transverse scans shows (a) uid- lled, dilated, hyperperistaltic segments of the small bowel and (b) a small microcolon (arrow) a b 401 Paediatric ultrasound Meconium ileus Meconium ileus is an obstruction in the nal ileum due to an intraluminal obstacle made up of meconium of anomalous consistency. Pellets of desiccated meconium are found in the distal ileum below a collection of viscous meconium in dilated loops. Generally, meconium ileus appears as a nonspeci c low obstruction and is di cult to di erentiate from low small-bowel atresia on clinical and radiological grounds. In distal small-bowel atresia, the microcolon opaci es quickly and there is a frank backward ow into the distal small-bowel loops. In meconium ileus, the colon lls slowly and with di culty to reveal the meconium pellets impacted in the distal ileum. Contrast enema is not always diagnostic, as there may be no opaci cation of the distal smallbowel loops due to perforation during lling. In order to con rm an organic obstruction, dilatation of all the small-bowel loops and marked microcolon must be demonstrated. Megacystis-microcolon-intestinal hypoperistalsis syndrome is syndrome consists of intestinal obstruction associated with nonobstructive megacystis, probably of myopathic origin. At the digestive level, there is a short small bowel, a microcolon, no or ine ective peristalsis and, frequently, malrotation. Clinically, the newborn presents with severe abdominal distension secondary to megacystis and failure to pass meconium. On ultrasound, the infant has a large bladder, o en with pelvic ureter and calyx dilatation. It results from antenatal digestive perforation, generally above an obstacle (atresia or volvulus). It evolves towards sterile plastic organization of the uid and the appearance of peritoneal calci cations. A capsule is formed by brous granulation, which is then calci ed and encircles the uid. Meconium cysts are sometimes found postnatally as an obstructive syndrome or abdominal mass. Plain abdominal lm and ultrasound are necessary and su cient to show cysts, peripheral calci cations, a microcolon and dilated small-bowel loops. Supine radiograph shows a large meconium pseudocyst with calci ed walls (arrows). Collagen bres, 85% of which consist of type I collagen, form the primary fascicles. Vascularization occurs through the musculo-tendinous junction, the periphery of the tendon and the enthesis (junction with the bone). Vascular tendons are covered by a single layer of synovia and loose areolar tissue, known as the paratenon, which contains the vessels that perfuse the tendons. Avascular tendons are surrounded by a synovial sheath composed of visceral and parietal lea ets connected by a mesotendon, through which vascular structures penetrate via the vincula. Only the long head tendon of the brachial biceps and the exor and extensor tendons located in the wrists, ankles, hands and feet are avascular. In normal tendons, lesions occur either at sites of biomechanical differences between tissues (the myotendinous junction or adjacent to bone) or in hypovascularized regions, which are considered critical, such as the third distal of the calcaneus tendon and close to the insertions of the supraspinal and brachial biceps tendons. Mechanical and vascular factors are implicated in tendinopathies, which are expressed histopathologically by the presence of tendinosis, corresponding to mucoid degeneration of the tendon, often accompanied by neovascularization, necrosis and dystrophic calcifications.
Queen of the Meadow (Meadowsweet). Nizagara.
- Are there safety concerns?
- Dosing considerations for Meadowsweet.
- How does Meadowsweet work?
- What is Meadowsweet?
- Bronchitis, heartburn, upset stomach, ulcers, gout, joint problems, bladder infections, and other conditions.
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96150