Aristocort
"Order 4mg aristocort with mastercard, allergy symptoms burning lips".
By: F. Miguel, M.B.A., M.B.B.S., M.H.S.
Professor, Rutgers Robert Wood Johnson Medical School
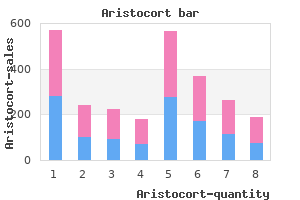
The local failure rates with T3 to 4 primary cancers are approximately 50% after combined modality therapy allergy testing macon ga discount aristocort on line. Because prognostic factors such as tumor size and lymph node status may be interrelated allergy shots xolair buy discount aristocort 4mg on-line, a multivariate analysis is required to determine if they are independent prognostic variables. Randomized Trials of Combined Modality Therapy for Anal Cancer T Stage: Univariate Analysis Salmon and colleagues found that size was significantly related to survival in a study in which radiation therapy alone was the primary treatment. In 95 patients treated with combined modality therapy plus brachytherapy there was an increase in 5-year colostomy-free survival with T1 and T2 tumors versus T3 and T4 tumors (T1, 83% and T2, 89%, vs. It must be emphasized that, unlike rectal cancer, inguinal lymph nodes in anal cancer are considered nodal metastasis rather than distant metastasis, and patients should be treated in a potentially curative fashion. In the historic literature, synchronous metastases to inguinal lymph nodes have been considered an indicator of a poor prognosis. Multivariate Analysis In the series from Allal and associates, factors by univariate analysis associated with a significant increase in local failure included age younger than 66 years, male gender, tumor extent more than one-third circumference, lymph node involvement, overall treatment time 75 days or greater, and the use of external-beam radiation for the boost treatment. Cloacogenic carcinomas have been considered to have a slightly better prognosis in some series 49,99; however, in 243 patients with resectable anal canal tumors, Papillon and Montbarbon reported a worse prognosis for patients with nonkeratinizing and basaloid carcinoma than for patients with keratinizing lesions. In one study, 61 grade was a significant prognostic factor, with low-grade tumors resulting in a 5-year survival of 75% compared with only 24% for high-grade tumors. By multivariate analysis, the 4-year local disease-free survival was significantly decreased in those patients whose tumors overexpressed p53 (64% vs. However, significant differences were not seen in disease-free or overall survival. In a retrospective analysis from the Princess Margaret Hospital, p53 was measured by immunohistochemistry in 49 patients who received combined modality therapy. By univariate analysis, p53 expression of 5% or greater was a poor prognostic factor for 5-year survival (78% vs. They account for 15% to 25% of all squamous cell cancers of the anus and, in general, have a different natural history and more favorable prognosis than squamous cell carcinomas of the anal canal. There is confusion in the literature as a variety of other definitions has been used, the most common being an area of skin measuring from 5 cm to as wide as 10 cm centered on the anal orifice. Cancers of the anal margin drain primarily to the inguinal lymph nodes, whereas cancers of the anal canal drain primarily to the inguinal as well as the internal iliac and superior hemorrhoidal nodes. Squamous cell carcinoma of the anal margin, as in skin elsewhere, has a favorable prognosis and rarely requires radical surgery. Wide local excision of these lesions is an attractive approach because it can be performed with primary closure and infrequently requires a split-thickness skin graft. The use of a wide local excision implies that an adequate margin of normal tissue (1 cm) can be secured beyond the tumor without anal incontinence. Local recurrence after primary treatment of anal margin cancers is routinely treated by repeat local excision. In the same study, four patients had an inguinal node recurrence as the only site of failure, and all underwent inguinal lymphadenectomy. Two of these patients were long-term survivors, one died of disease, and one was lost to follow-up. Squamous cell carcinoma of the anal margin tends to be early or only moderately advanced at the time of diagnosis. Lymph nodes are rarely involved (0% to Although early cancers of the anal margin are successfully treated by local excision, nonoperative treatment should be considered for some patients. Papillon suggested that radiation therapy should be used for patients with anal margin carcinomas that are considered unresectable or patients who have extensive or recurrent lesions; in addition, patients who are medically inoperable may be able to have radiation therapy. Selected series reporting the use of primary nonoperative therapy for anal margin cancers are seen in Table 33. Patients received radiation therapy (external beam with or without brachytherapy) or combined modality therapy. The numbers of patients in each series are small, making it difficult to make definitive conclusions.
Diseases
- Mitochondrial trifunctional protein deficiency
- Retinopathy, arteriosclerotic
- Chickenpox
- Hypertrichosis, anterior cervical
- Mental retardation unusual facies talipes hand anomalies
- Upper limb defect eye and ear abnormalities
In contrast to the endocrine syndromes allergy shots ogden utah aristocort 4mg mastercard, for which successful treatment of the tumor effectively controls the symptoms allergy shots immune system 4mg aristocort with amex, the severity of the neurologic symptoms is unrelated to tumor bulk and often does not improve despite successful antineoplastic therapy. The Lambert-Eaton syndrome is characterized by proximal muscle weakness that improves with continued use and hyporeflexia and dysautonomia. The cause is related to autoantibody impairment of acetylcholine release from the cholinergic nerve terminals. Surgery plays a minor role in the management of this disease, and less than 10% of patients might be considered candidates for thoracotomy. These sites include an ipsilateral pleural effusion, supraclavicular lymphadenopathy (ipsilateral or contralateral), or contralateral mediastinal lymphadenopathy. In an analysis of two large cooperative group databases, which included in toto more than 4000 patients, the survival of patients with an isolated effusion was similar to patients with one site of extensive disease. It is assumed that these effusions are malignant, unless the fluid is a transudate, nonhemorrhagic, and cytologically negative on repeated examination results. Clinical judgment in individual cases should be applied for selection of these patients for combined modality therapy until this issue is addressed in a prospective trial. The presence of supraclavicular lymphadenopathy is commonly associated with extensive disease, but when encountered in patients with otherwise limited disease (5% of cases), carries a trend toward poorer survival. However, two randomized studies that evaluated the use of a more aggressive, twice daily, radiation regimen, excluded patients with contralateral hilar disease, 69,70 presumably to reduce the volume of irradiated field and the risk for toxicity. If this form of more intensive radiotherapy becomes a standard of care, the potential prognostic significance of the extent of mediastinal nodal involvement will need to be reexamined. Patients with limited-stage disease who present with superior vena cava syndrome have a similar prognosis to other patients with limited-stage disease 62,71 and have been included in randomized studies investigating the role of combined modality therapy. Patients who undergo surgical resection and have an absence of mediastinal metastases have an especially favorable outcome. Among the patients with extensive disease, a number of studies have shown that the number of metastatic sites is an important parameter. Performance status reflects both the underlying extent of the disease and partially dictates tolerance for the intensity of treatment. Although patients with a lower performance status are at a higher risk for treatment-related complications, they may still benefit from a combined modality approach. In some large cooperative group trials, treatment-related mortality has exceeded 10%. Several retrospective analyses have attempted to identify patients at increased risk for a treatment-related mortality. An analysis of 382 patients treated in a single institution identified age older than 50 years, Karnofsky performance status less than or equal to 50, treatment with a regimen containing three drugs or more, and a prior septic episode during chemotherapy as risk factors for septic complications. The Copenhagen Lung Cancer Group compared 937 patients treated in its two most recent studies with 819 patients treated in early clinical studies. Based on this algorithm, 21% of the 937 patients would be considered at high risk. In this high-risk group, the median survival time was 133 days, and the 2-year survival was 4. Mortality during the first chemotherapy cycle was 33%, and among patients treated with etoposide and platinum the frequency was 41%. For these high-risk patients, therefore, less intensive chemotherapy would be appropriate, and careful monitoring and support during treatment is mandatory. Exceptions would include the presence of additional symptomatic areas that may require prompt therapy, such as symptoms and signs suggestive of metastases to a weight-bearing bone or the neuraxis. In an era of cost containment, algorithms have been proposed that use each diagnostic modality in a stepwise fashion to reduce the costs of the staging workup. However, its capability to assess tumor response is limited in areas of atelectasis and radiation-induced fibrosis where the presence of active tumor cannot be ascertained. If asymptomatic brain metastases are present, chemotherapy may be adequate treatment,110 and the early detection and treatment of asymptomatic brain metastases with radiation therapy has not been shown to significantly improve patient outcome, 107,109 partly due to the effect of systemic failure on survival. If brain metastases are the single site of distant disease, the prognosis may not be significantly altered because the median survival compared with patients with limited disease has been comparable in some series, 111,112 although not in others.
The authors recommended that treatment of indeterminate lesions be treated as primary lung carcinomas allergy treatment breakthrough order cheap aristocort on line. Pulmonary metastases from sarcomas or other distinctive nonpulmonary neoplasms are usually easy to diagnose allergy qld buy cheap aristocort 4 mg on-line. A generous wedge excision or lobectomy and mediastinal lymph node dissection should be performed. Traditionally, a comparison of the primary neoplasm and the lung nodule using light microscopy has been the only method for determining origin of the lung nodule or neoplasm. Electron microscopy137 or specific molecular or genetic characteristics may identify more precisely the origin of such neoplasms. Monoclonal antibodies can assist in discriminating between primary bronchogenic adenocarcinoma and colon carcinoma metastatic to the lung. Characteristics of metastases and of primary lung carcinoma were examined in an attempt to better direct subsequent therapy. Patients with pulmonary metastases may undergo multiple procedures for re-resection of metastases, with prolonged survival after complete resection. Several studies have reviewed results of multiple resections for recurrent pulmonary metastases. Thirty-four patients were resectable (median survival, 28 months; 5-year survival, approximately 32%). Survival after resection of a solitary recurrent metastasis was 65 months (median) compared to patients with two or more nodules (median, 14 months; P =. At the National Cancer Institute, 70 patients underwent at least one reoperation between 1965 and 1995. The authors noted that complete resection was the most important and favorable prognostic factor. Patients with complete resection had improved survival compared with those who were incompletely resected. Fewer than 3% of all patients undergoing resection of pulmonary metastases will require an extended resection. Pneumonectomy or en bloc resection of pulmonary metastases with chest wall or other thoracic structures, such as diaphragm, pericardium, and superior vena cava, have been performed in a small number of patients with good results. Mortality was 5% and occurred in those patients having pneumonectomy often after multiple prior wedge resections for metastases. The need for pneumonectomy may be evident in the large metastases that involve the majority of one lung and that compress the heart and shift the mediastinum (. In a French study of 42 patients treated over 10 years, 146 29 patients underwent pneumonectomy for sarcoma; 12 for carcinoma; and one for a lipoma. Two postoperative deaths occurred, and four patients had major complications; five patients (12%) had recurrences in the residual lung. The standard surgical mortality for operations for pulmonary metastases is less than 1%. Patients with large centrally located metastases may require pneumonectomy for complete resection. Although mortality for pneumonectomy for pulmonary metastases corresponds to mortality for other histologies, the 5-year survival rate of only 16% demands careful selection of patients before resection. A: Chest roentgenogram with a massive pulmonary metastasis from malignant fibrous histiocytoma compressing and shifting the mediastinum into the contralateral hemithorax. Impairment of ventilation to the involved hemithorax and secondary compression of the contralateral hemithorax further impairs ventilation. B: Chest computed tomography with a massive pulmonary metastasis from osteogenic sarcoma compressing the superior vena cava, right heart, and right lung, and shifting the mediastinum into the left chest. Resection often requires extracorporeal support to allow decompression and manipulation of the heart and pulmonary veins. An approach to the right pulmonary artery and veins and the right mainstem bronchus via a median sternotomy allows for control of the pulmonary vasculature and airway before removal of the tumor. The value of pneumonectomy was also examined by retrospective review of the International Registry of Lung Metastases.
Disease occurs more frequently in male than in female subjects (2:1 ratio) and primarily involves individuals in the sixth decade of life allergy medicine under the tongue discount aristocort 4mg on line. It is noted that cancer of the paranasal sinuses is more frequently observed in other regions of the world including Japan and South Africa allergy shots and kidney disease buy aristocort 4 mg otc. The nasal vestibule is the triangular region of the nasal cavity bounded by the palatine processes of the maxilla inferiorly, the nasal septum medially, and laterally by the fibrofatty tissue called the nasal ala. The nasal vestibule represents that portion of the nasal cavity composed of skin. The nasal antrum represents the remaining portion of the nasal cavity and contains the inferior, middle, and superior turbinates. The superior and middle turbinates are composed of highly vascular tissue overlying fragile bony projections that inset onto the ethmoid air cell bony framework. The paranasal sinuses include the maxillary, ethmoid, sphenoid, and frontal sinus. The ethmoid sinuses drain into the submandibular as well as retropharyngeal nodes. The nasal cavity drains into these regions as well as along the course of the facial blood vessels into the submandibular triangle and to periparotid nodes. Distinct from other sites within the upper aerodigestive tract, however, squamous cell carcinoma is less predominant. Tumors found in the superior portion of the nasal cavity include adenocarcinoma and esthesioneuroblastoma. In the paranasal sinuses, additional neoplasms include tumors of minor salivary gland origin including adenocarcinoma, adenoid cystic carcinoma, and mucoepidermoid carcinoma. Rare tumors of this region are lymphoma, mucosal melanoma, teratocarcinomas, angiosarcomas, and various odontogenic and bone tumors. Common presenting symptoms include a nonhealing ulcer, occasional bleeding, and unilateral nasal obstruction. Given the anatomic limitations in making early diagnosis, disease is usually far advanced at time of initial presentation. Other symptoms may reflect growth into the oral cavity causing dental pain, loose teeth, or ill-fitting dentures, or into the orbit leading to ocular symptoms such as diplopia, proptosis, and epiphora. Tumors in the superior nasal antrum and paranasal sinuses may invade the cribriform plate and extend into the anterior cranial fossa, causing anosmia or headache. The regional lymph nodes most frequently involved with metastatic disease are nodes within the periparotid region or within the submandibular triangle. The propensity for spread to regional lymph nodes is dependent on the subsite in which primary disease may occur. Regional lymph node spread is less frequently seen from tumors of the ethmoid and maxillary sinus, approaching 10% to 15% of patients. The probability of lymph node spread increases with extension of tumors outside the normal confines of the nasal and paranasal cavities, especially with extension into the oral cavity. Prognoses from nasal cavity lesions are directly proportional to size of the lesion and overall approximate 60% at 5 years. Prognosis for paranasal sinus cancers likewise depends on extent of primary disease at presentation and approximates 30% for advanced T4 lesions. The regional lymph node (N) and distant metastases (M) staging are identical to other sites within the upper aerodigestive tract and are as stated previously (see Staging, earlier in this chapter). Staging for Cancer of the Maxillary Sinus Careful examination of patients presenting with symptoms referable to the midface may minimize delay in diagnosis of these cancers. Likewise, considerable progress has occurred in the use of diagnostic radiology in the preoperative assessment of tumors of this region. Coronal computed tomographic scan demonstrating bony involvement of the lamina papyracea (curved arrow) and intracranial extension (double arrow). T1-weighted sagittal magnetic resonance image showing dural invasion (arrows) within the same patient as in Figure 30. Tumors of the nasal septum can be approached through a lateral rhinotomy or by a midface degloving technique. Wong and Cummings have pointed out that most patients presented with lesions that are less than or equal to 5 cm, and less than 10% present with lymph node metastases. Given the high propensity for local recurrence, combined modality therapy consisting of surgery and radiation should be used in most circumstances.
Purchase aristocort online now. What is allergen immunotherapy? | facingallergies.com.